Waystar
About Waystar
Waystar Pricing
Please contact Waystar for pricing details.
Free trial:
Not Available
Free version:
Not Available
Other Top Recommended Medical Software
Most Helpful Reviews for Waystar
1 - 5 of 199 Reviews
Carmen
10,001+ employees
Used less than 2 years
OVERALL RATING:
4
Reviewed December 2021
Waystar After a Year...
Marlo
Hospital & Health Care, 2-10 employees
Used daily for more than 2 years
OVERALL RATING:
5
EASE OF USE
5
VALUE FOR MONEY
5
CUSTOMER SUPPORT
5
FUNCTIONALITY
5
Reviewed September 2022
Great Software for Great Price
great software and very happy with customer service
PROSVery user friendly for both the clinical and office staff
CONSwould like to see all doc information interchangeable if wrong doc was utilized
Reason for choosing Waystar
user friendly for all staff needs
Reasons for switching to Waystar
not user friendly
Mike
Hospital & Health Care, 11-50 employees
Used daily for more than 2 years
OVERALL RATING:
5
EASE OF USE
5
CUSTOMER SUPPORT
5
FUNCTIONALITY
5
Reviewed January 2019
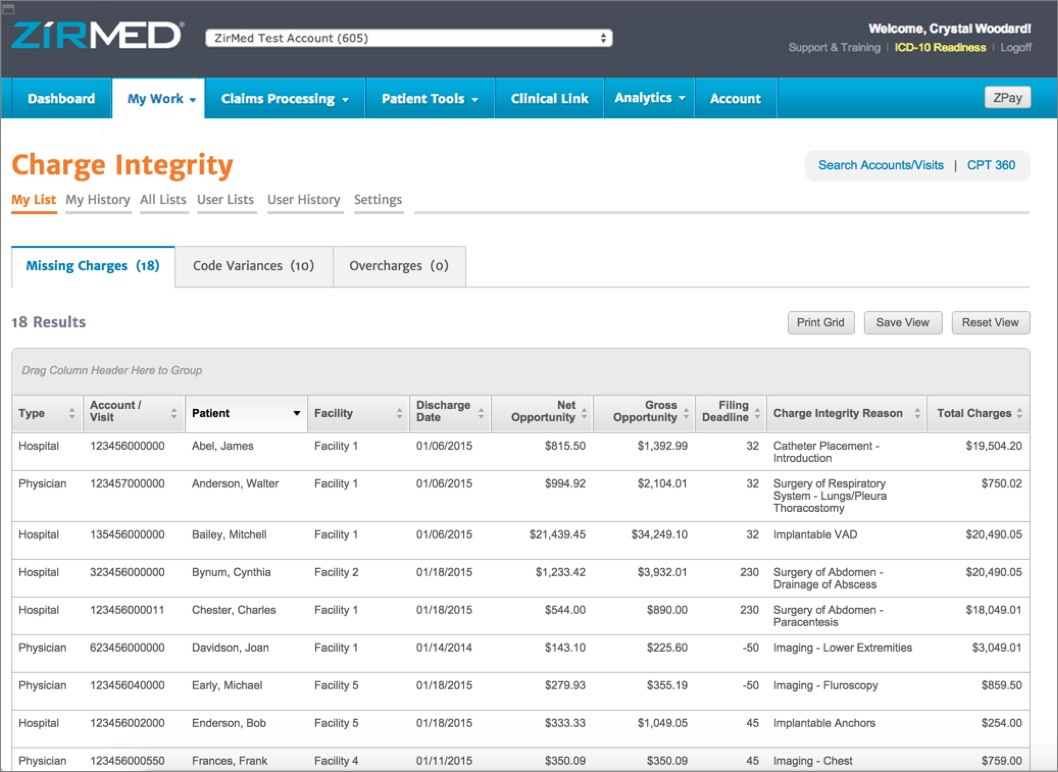
Waystar (Formerly Zirmed)
Before we got Waystar (Zirmed), we would either submit the claims on paper (which is hard to track) or through the payers provider portal. We would need to maintain a dozen or so username and password for various websites. You would need to sign up for a lot of websites. With Waystar, all you need is one username and password. You can electronically submit claims to various payers with one click. Waystar will scrub the claim to see if there are any front end rejections. If the payer rejects the claim, you can correct it within Waystar without having to go back to the EMR and correct it. You can track your claims within Waystar. You can download an excel spreadsheet with the information you need.
PROSYou have the ability to correct claims that get rejected by the insurance company. Waystar will scrub your claims even before they sent it off you the insurance company. The layout is very user-friendly and straight forward. If the Payer allows it, remittance advice can be downloaded and uploaded to the EHR software. Claims can be copied if you have to enter them manually. YOu don't need to reenter the whole patient information over and over again.
CONSYou'll need to call in order to add a child account. The claims status should be updated if the claim has been paid. Right now, the last status you'll get us if the claim is recieved by the Payer.
Carrie
Hospital & Health Care, 1 employee
Used daily for more than 2 years
OVERALL RATING:
1
EASE OF USE
1
VALUE FOR MONEY
1
CUSTOMER SUPPORT
1
FUNCTIONALITY
1
Reviewed April 2020
Choose Another Company...much better options out there than Waystar
I haven’t been happy with the service when they were NAvicure or Waystar.
PROSI didn’t feel that their software was very useful.
CONSThe company is costly. There clearinghouse isn’t very effective with all insurances. I had to manually bill some insurances since their clearing house couldn’t do it. They charge you extra to find out about denials. When you have issues, you can’t reach customer service well. There customer service isn’t good with getting back to you. When you leave their service, they require 90 notice to get there money. When you give notice on April 24, they cancel you on 7/30 to get as much money as they can. By the way, my renewal date was June 1, but they still made me go to 7/30 to pay them. When asked to talk to a supervisor, [SENSITIVE CONTENT HIDDEN] in Customer Relations kept telling me that I had to pay up to 7/30 or could pay all 90 days fees now to be done on 4/30. I asked 3 times for a supervisor and didn’t hear from anyone. They just want money and don’t care about their customers.
Reason for choosing Waystar
It seemed ok at the time.
Reasons for switching to Waystar
Cost effective; telehealth; easy to use; great customer service
Brenda
Medical Practice, 2-10 employees
Used daily for more than 2 years
OVERALL RATING:
5
EASE OF USE
5
VALUE FOR MONEY
5
CUSTOMER SUPPORT
5
FUNCTIONALITY
5
Reviewed May 2020
Great product for a great value
We started with Zirmed and transitioned to Waystar. It was flawless. It's easy to use. The value is excellent. They have a huge list of insurances OR you can have them send a paper claim. We were working with an older (outdated, frankly) practice management software and Waystar worked with us so we could still upload claims. Editing rejected claims is very easy. There are also Premium products you can buy if you would like to streamline your RCM such as code look up and insurance verification.
PROSIt is very user friendly. Their customer service has always been very responsive.
CONSMedicare Secondary billing is clumsy. (Not a Con but) there are several features we don't need/use. They clutter up the dashboard.
Reason for choosing Waystar
I was pleased by the price, the functionality it offered, and the sales/tech people were wonderful and weren't pushy.
Reasons for switching to Waystar
We weren't unhappy with Proxymed but we felt it wasn't outstanding. I'd heard great reviews about Zirmed from several colleagues. I looked into it. We ended up paying less than Proxymed and there were more features with Zirmed (this was 10+ years ago).