Dealing With Difficult Patients: Strategies for Healthcare Professionals
Practice managers and owners are the front line defense against dealing with difficult patients, so it’s crucial to develop effective strategies in order to handle complicated patient interactions. Understanding the different types of difficult patients you might encounter will help you develop a plan that can promote a positive, productive clinical environment for your staff while also minimizing the risk of patient attrition.
Practice owners and managers who are practiced in remaining empathetic and understanding of patient concerns are more likely to minimize the risk of negative reviews and increase patient retention because they are able to diffuse difficult patient interactions with more aplomb and tact.
We surveyed real doctors in order to find out the most common types of difficult patients that they have encountered. We also spoke with Dr. Gerda Maissel, a Board Certified Patient Advocate (BPCA) and Board Certified Physical Medicine and Rehabilitation (PM&R) physician with over 30 years of experience. [1] She has shared with us some of the strategies that she found most useful for improving patient loyalty during her years managing a healthcare organization.
Dr. Gerda Maissel
Different types of difficult patients doctors often deal with
According to the Software Advice 2023 Patient Wait Times Survey*, a majority of doctors had to dismiss at least one patient due to their conduct in the last two years.
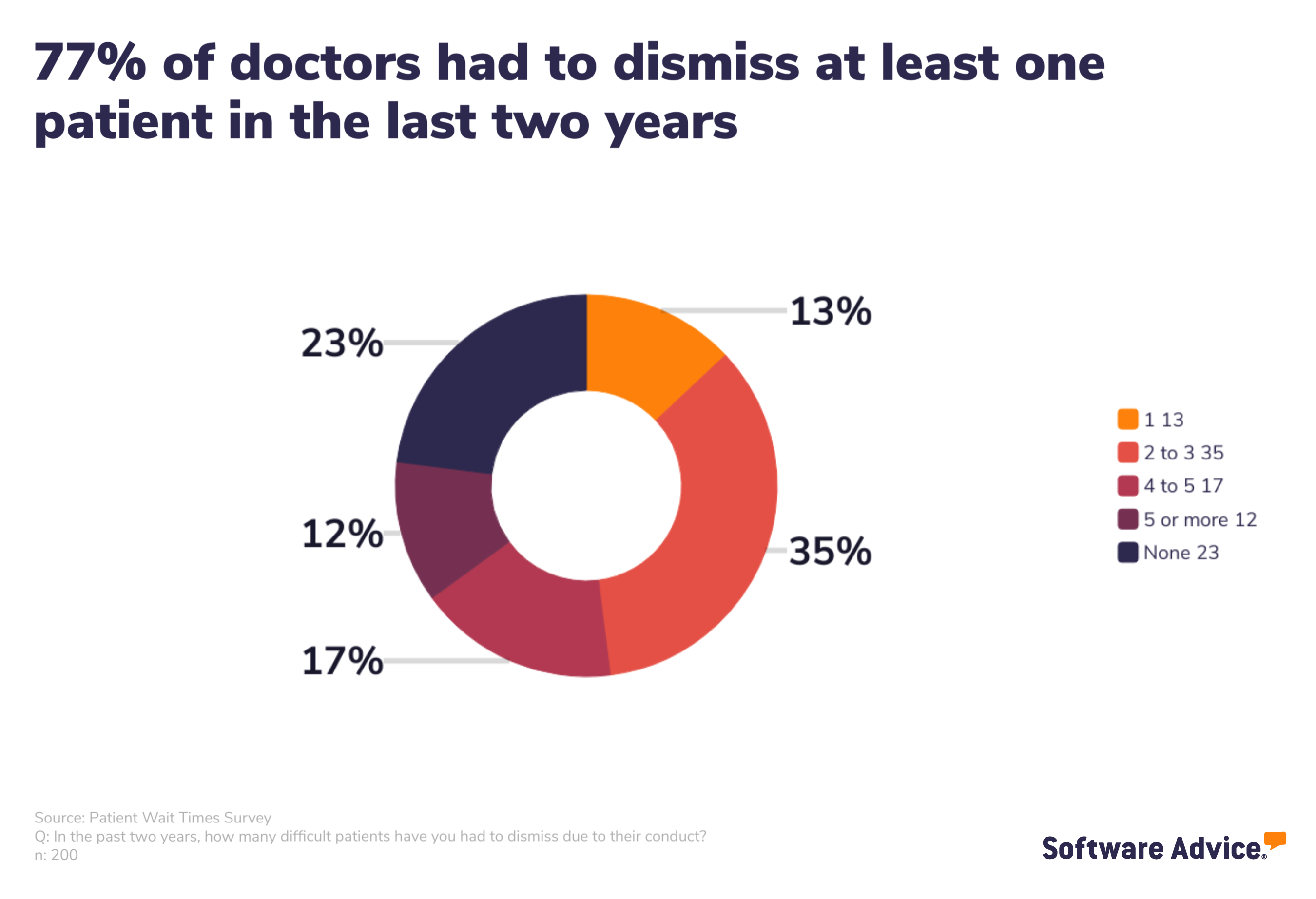
Of the patients who were dismissed, the overwhelming majority of them were dismissed due to inappropriate or disruptive behavior. That makes sense because when you think of a difficult patient encounter, your first thought probably goes to that patient that made your staff’s lives more difficult than it needed to be.
But that behavior can go beyond just influencing your staff. If other patients in the waiting area or exam rooms hear the exchange, it can negatively affect their experience, which can further impact patient retention.
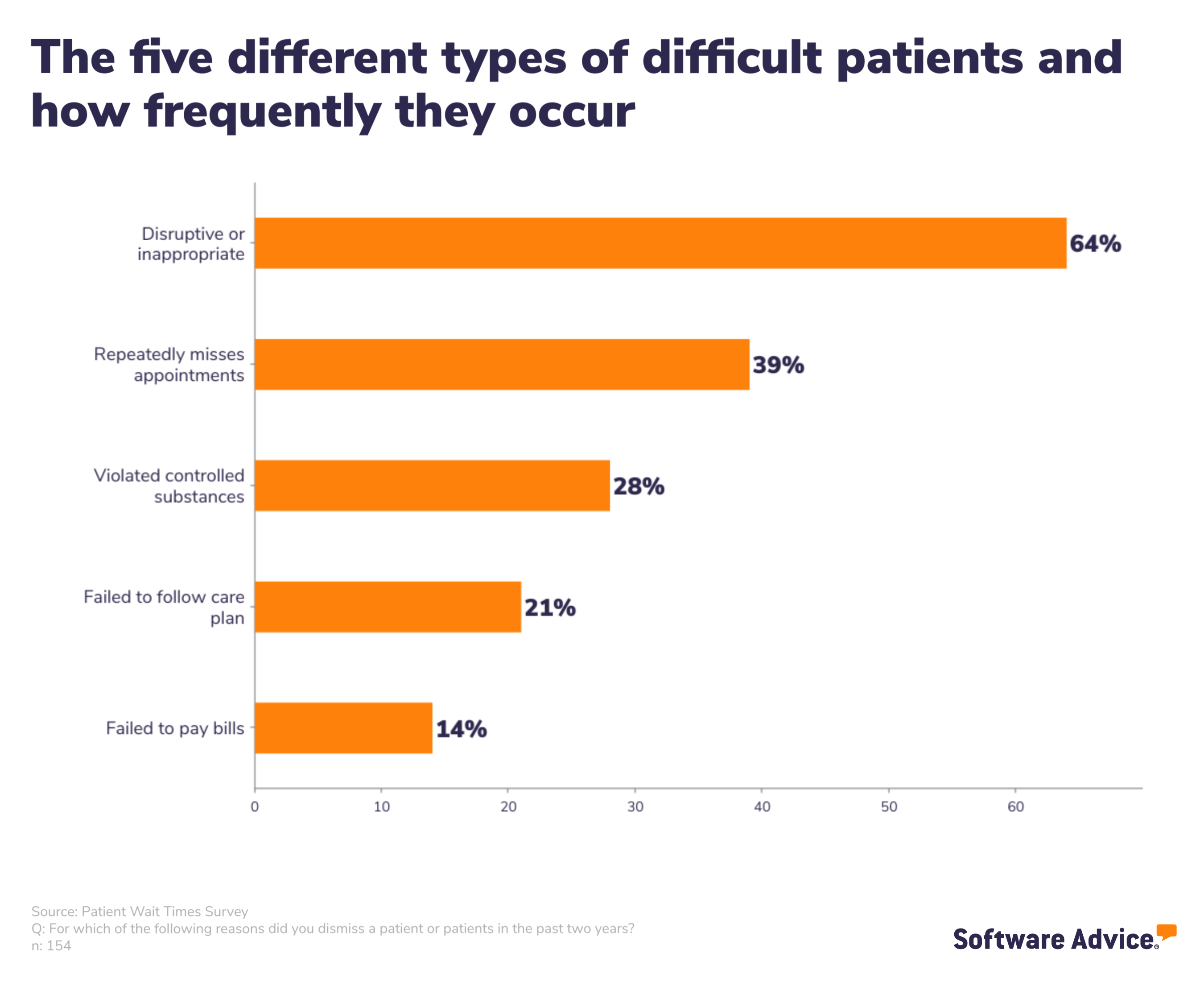
And while dealing with inappropriate or disruptive patients should be a focus, it might not be the problem you’re having. You need to have strategies to deal with all types of difficult patients to ensure you, your staff, and your patients can all work together to ensure that the practice runs smoothly and everyone gets the care and attention they need and deserve.
Patient type: Disruptive and inappropriate patient
Because dealing with disruptive or inappropriate patients is the most significant pain point faced by a healthcare professional, we’re going to break down the different strategies you can use to alleviate some of the tension before you have to take the extreme measure of dismissing them.
Strategy #1: Listen to patient concerns in good faith
The first step to dealing with a challenging patient is to patiently listen to their concerns in good faith. Pay attention to what they’re worried about to find the best solution to their problem. They’re angry or upset for a reason, and even if you think that reason isn’t justified, that doesn’t make them any less upset.
Your patient is upset for a reason. It might be frustration with their illness or injury or something unrelated to what’s happening in your office. That’s why you have to approach each situation with compassion and understanding.
As a practice owner or practice manager, it’s your job to be the umbrella for the rest of your staff. You need to get in front of difficult patients whenever possible to shield your staff from the worst of it. This might mean that you need to step in quickly to diffuse situations.
Dr. Maissel
It’s about listening and being proactive in your response. Acknowledge their problem and apologize for it. This helps build rapport and trust with the patient and shows that you are willing to fix their trouble.
Strategy #2: Set boundaries to protect your staff
Know what thresholds and boundaries you want to enforce before problem patients act on them. Above all, you want your staff to feel like they’re working in a safe environment, so having a no-tolerance policy on sexual advancements or threats means that you sometimes need to let go of a patient without hesitation.
You might have a warning system to let the patient know that what they were doing is inappropriate, and if they continue to act that way, they will be asked to find a new provider.
Establishing office policies can help manage difficult patients by creating fair, unbiased procedures for your staff to follow if a patient becomes disruptive or misbehaves.
You can set rules regarding patient behaviors, from aggressive acts or speech directed toward you or your staff to failure to make payments. When coming up with your management, consider the following:
Are there degrees of severity to the type of patient behavior a rule aims to prevent? Or will the simple act of breaking a rule result in your practice taking action? What patient behaviors do you find most disruptive in your practice?
For example, Would you consider a patient's failure to pay bills enough to fire them? Or are there more pressing issues that you’d be more concerned with addressing first, such as prescription abuse?
Once you’ve worked out your rules, you’ll need to devise a set procedure for your team to follow when a patient violates one or more of these policies. Determine what patient behavior triggers the procedure, and train your staff on exactly how to handle these situations.
Dr. Maissel
Strategy #3: Be creative with your solutions
When you genuinely listen to a patient’s concerns, you might see what’s the problem. They might be complaining about one thing, but really, they want more time with their doctor, or they might want something done slightly differently. They might think a particular doctor doesn’t have their best interest at heart, even if it’s false.
You need to be creative with your ability to problem solve by offering the most simple solution that will solve their problem.
If a patient is unhappy with their provider, allow them to switch to another one in your practice if that’s available. You have all of their information in your system, so it wouldn’t be a difficult solution while also making them feel heard.
Case story
We had a patient driving our staff crazy because they would often come to the emergency room. This patient was becoming costly to our organization and was being disruptive. The first thing we did was set aside time to talk to them to figure out what made them so anxious about their medical conditions.
We discovered they were afraid they wouldn’t be able to get appointments whenever they felt they needed them, so they resorted to the emergency room instead. We solved this problem by sitting down and scheduling a weekly appointment for them and their doctor so they would feel heard.
They got the attention they sought, and their consistent visits didn’t tax our emergency room staff. Eventually, the emergency room visits stopped, and they even cut back to monthly visits instead of weekly because they felt like they had more control over their medical conditions.
Patient type: Repeatedly misses appointments
You and your staff build your day around the scheduled appointments, so when a patient doesn’t show up, it can be disruptive and costs your practice revenue. It’s a frustrating problem that can throw entire days out of whack, but luckily, there are some relatively easy solutions to help alleviate the issue.
First, it’s important to understand why your patients might be missing these appointments. If an appointment is just flat-out missed, it’s more than likely that they forgot about it. They might have scheduled it weeks ago and didn’t put it into their calendar.
If a patient is often late to appointments--an equally disruptive behavior--it might be because they have a disability and have trouble getting to your office. They might rely on inconsistent transportation options that are out of their control.
That’s why it’s so important to empathize with your patients and offer them solutions to their concerns before you go to the extreme of dismissing them.
Strategy #1: Use automatic reminders with appointment reminder software
It’s pretty standard practice to remind patients about their appointments, but in the past, this relied upon members of your staff to manually call every patient who was scheduled to come in the following day. This could often take hours that would have been better spent doing something more productive.
Appointment reminder software can help you remind patients about upcoming appointments via phone call, text message, or email at specified dates and times before the appointment.
During intake, it’s essential to ask your patients which way they prefer to be contacted about appointment reminders. Younger patients likely won’t answer a phone call from an unknown number, while older patients might miss an email or text reminder.
If patients opt-in, they’ll receive automatic reminders for their appointments. You can set these up so that they get sent at certain times. You can send a reminder a week out and another the day before.
Include the time of the appointment as well as your office address. If you have general directions about how to get to your office on your website, include a link to that as well.
Strategy #2: Have a plan for patients who miss or are late for appointments
There are a few different solutions to no-shows or late appointments that you can take with your patients to deter them from occurring. During intake and after each missed appointment, you will need to let your patients know about the expectations.
If you have a three-strike policy, let your patients know the first time they come in. Call them after their first missed appointment to remind them. In most cases, patients don’t want to miss their appointments. During that conversation, talk to them about why they missed their appointment. If they missed it because they forgot, remind them of your policy and reschedule them for a later date.
If extenuating circumstances prevented them from attending, you might be more lenient. Encourage them to call the next time something happens that will prevent them from attending so that your office can adjust their schedule.
Another solution is to charge a small fee for no-shows as a deterrent. Again, communicate with your patients upfront about this policy so they aren’t taken off guard. This method comes with unique challenges, according to Dr. Maissel:
Dr. Maissel
A strategy that Dr. Maissel found helpful was to flag patients who were frequently late in your system and create a specific day where, instead of set time slots, there would be a chunk of time that these patients could come in.
So, from noon to 5 p.m., this group of patients could arrive whenever they wanted and would be seen in order of arrival by a doctor. She found it an effective way to accommodate patients who might have trouble getting to their appointments on time.
Patient type: Failing to follow medical recommendations
Patients who fail to follow their care plan can be frustrating, and it can be hard knowing if a patient is just obstinate and will never follow their care plan or if you can find a solution that will work.
Just because a patient consistently makes choices that go against their care plan doesn’t mean that they should be dismissed without attempting to find a solution to their problem. That’s where strategies such as remote patient monitoring can come in handy.
Suppose a patient who has a chronic care condition like diabetes isn’t following their diet. In that case, remote patient monitoring can help your patient stay on track. Remote patient monitoring is a healthcare delivery model that uses tech to monitor patients’ health outside your clinic or practice.
It can include everything from digital blood oximeters that will alert you if something is abnormal to blood glucose monitors that are synced up to an app that will monitor spikes in blood sugar levels.

Dexcom’s glucose monitoring devices [2]
When you equip patients with the ability to monitor their health at home, they’ll see the short and long-term effects of their decisions on their health instead of only thinking about them during their appointments.
If they still don’t follow their care plan even after implementing solutions to help them manage it, then you can begin to have difficult discussions about why they might not be an effective fit for your practice.
For more information about remote patient monitoring and how you can implement it in your practice, check out these resources:
Patient type: Potential substance abuse problems
Discussing potential substance abuse problems with patients can be awkward and difficult. According to Dr. Maissel, the first step is to create a safe environment where they feel comfortable with you and trust you not to judge or report them.
Dr. Maissel
Strategy #1: Create a safe, judgment-free environment
If you suspect a patient has a substance abuse issue, your first priority is to get them the medical help they need. This starts by having open and honest communication. It would help if you let your patients know that they will not be judged and let them know upfront that your only goal is to help them get the medical attention they need.
Strategy #2: Test patients whom you suspect to get more information
In addition to establishing that safe space, you also have to test patients you suspect might have substance abuse problems because it’s important to understand not only what substances they have so that you can make a more informed decision.
Let your patient know that it’s crucial that you have as much information possible because, without it, you might prescribe something that will interact with what’s in their system in a negative way.
Additionally, suppose you’re prescribing narcotics, and it’s going to be more than just a one-time script. In that case, you should ensure that your patients are signing a narcotic contract, which ensures that they will receive random drug tests to ensure they are taking the medication and not abusing it.
With all that said, if you have a manipulative patient or one which refuses to trust you and takes a drug test while also conveniently losing their medication regularly, you must still use your best judgment. If they aren’t willing to work with you, you still need to be able to dismiss them; try to work through their problems as much as possible before you take that step.
Patient type: Failing to pay medical bills
Failure to pay medical bills might be the trickiest of problems to handle as a practice owner or admin because you’re often not the one in charge of collections. That said, you can still implement solutions in your practice that can help.
Strategy #1: Increase the number of ways patients can pay you
The more ways that you have that will allow patients to pay you, the more likely they will be to do it. Often, patients will need clarification about where/how to pay you after a procedure. Do they pay after it’s done? Do they wait to get a letter in the mail? Will you send an email?
Communicate with your patients about what bills they might receive early and often. Let them know that they’ll receive separate bills for different parts of a procedure. Have your staff break down everything they might get contacted about.
Will they be charged separately for any testing that you send out for? How about anesthesia? Often, patients won’t know they won’t get one bill, so they will think they’ve already paid for it.
You can also lower the barrier of confusion by setting up text reminders that make it easier for patients to pay from their phones. The text can include a link to the bill, information about the costs, and a place where they can easily pay it.
Another solution might be to have a place where patients can immediately pay in your office. It will never be more top of mind than while they are there.
Strategy #2: Communicate with your coders
One of the pain points that can stop patients from paying is if their procedure gets rejected by insurance even though it shouldn’t have. This might stem from a miscommunication between your doctors and your coders. If a coder receives the wrong code, insurance won’t know what to bill, and it will get rejected.
That’s why, as a practice owner or practice manager, you need to encourage your doctors and staff to develop effective relationships with the coders. Encourage them to respond to coder inquiries as soon as possible so that billing can be accurate and you can avoid headaches down the line.
Dismissing patients should be a last resort when dealing with difficult patient
Your patients are human and their stresses can sometimes bleed over into your practice. That’s why it’s important to have a bevy of strategies to better handle whatever difficult situation you might face. Whether that’s a patient who is stressed and short-tempered, someone who you are concerned might be abusing a substance, or a patient who absent-mindedly missed their appointment for the third time, you need to have a strategy in place.
These strategies outlined above are great general advice, but each and every situation will be different because each person is different. That’s why the most important strategy is developing and honing your communication skills to adapt and handle any situation thrown at you.
For more information about how to improve your patient communication strategies, check out these other resources:
Survey methodology
The Software Advice 2023 Patient Wait Times Survey was also conducted in March 2023. It polled 500 patients in the U.S. who had seen a healthcare provider, including general practitioners, specialists, and mental health providers, within the last two years.