What You Need To Know About the Different Types of Medical Practice Payment Models
If you’re a doctor starting your own practice and are wondering which healthcare payment model will be the right fit for your practice, knowing which models are available for you and understanding the pros and cons of each is a good place to start. Choosing the right one will help you maximize your profitability while maintaining your preferred level of patient interaction.
To make the best decision for your new practice, you have to consider several factors:
How you want to make your revenue
How many patients you want to service
How much you need to track metrics
How much coding and billing you need to worry about
We’ll be going over all of these factors and more by providing you with a detailed breakdown of several different healthcare payment models: Fee for service, concierge medicine, direct primary care (DPC), and value-based care. We’re also including insights that are informed by Gartner research, as well as an interview with an expert for concierge medicine, Terry Bauer, CEO of Specialdocs [1].
Fee for service is the most traditional and most prevalent payment model
In the fee-for-service model, doctors and healthcare organizations get paid strictly based on the individual care services they provide. It’s the most traditional pricing model used in healthcare because it’s easy to quantify metrics for billing purposes which makes getting paid for services much easier.
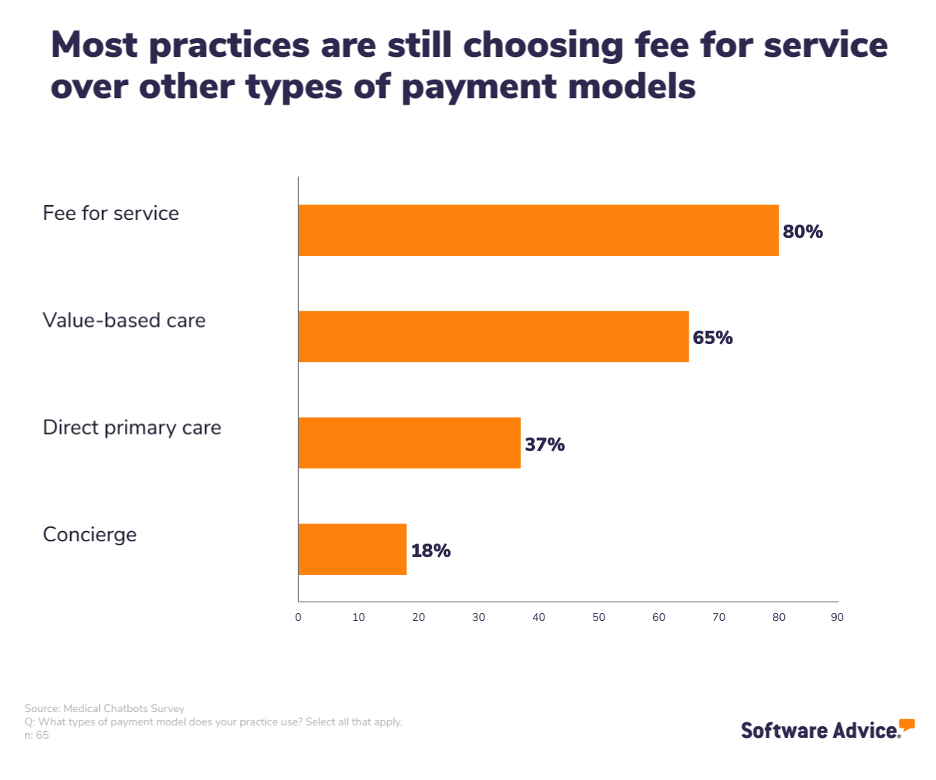
Our recent Software Advice Medical Chatbots Survey* shows that most of your colleagues are still using a fee-for-service model.
Using the fee-for-service model, a healthcare provider charges based on individual services such as appointments, treatments, tests ordered, and prescriptions given, then lists all of these services separately on a bill which can often be long and confusing for the patient.
Pros and cons of fee for service
Pros:
Coding and billing is very straightforward: Billing is easier for healthcare providers because of the straightforward nature by which they receive their payments.
Patients know what to expect: For basic services, fee for service is a relatively simple and straightforward method for patients because the billing process for doctors and administrators isn’t complicated.
Metrics are easier to track: Metrics are also often easier to track because you can easily quantify the number of services you are providing and know how much each of those services cost. It makes the billing process significantly easier to track as well.
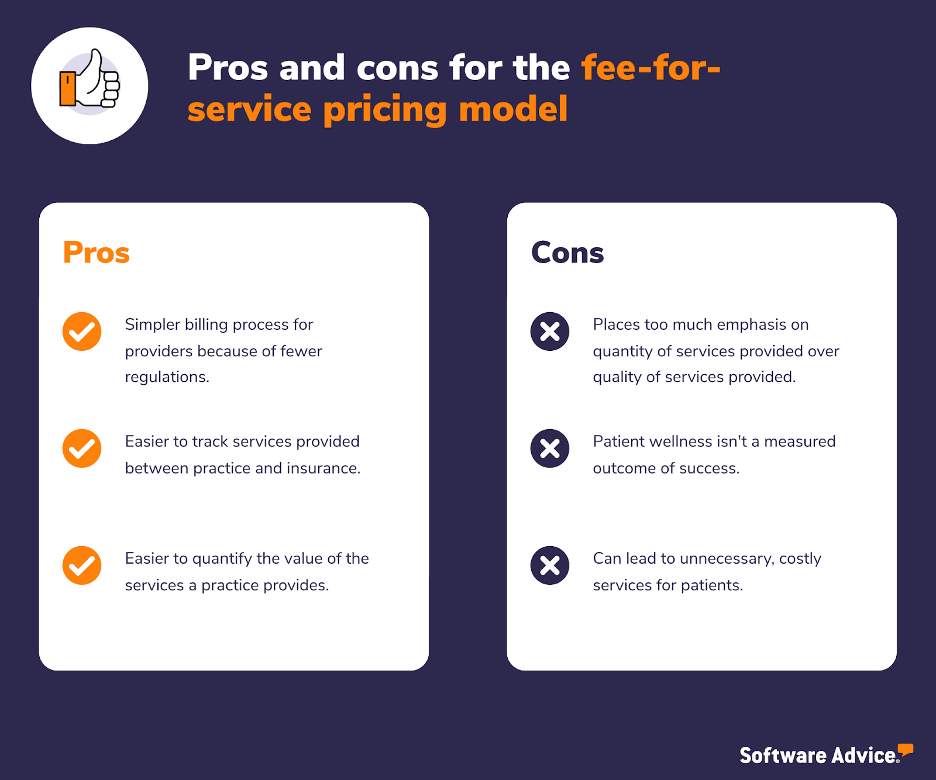
Cons:
You are incentivized to take on more patients than you might be able to handle: Due to the quantity-over-quality environment, this payment method incentivizes a provider to take on as many patients as they possibly can in order to make the most money. This could mean less patient satisfaction and less positive care outcomes.
You have less time with your patients: Physicians spend less one-on-one time with the patients and prescribe more tests without getting to the root of what patients may be experiencing, thus impacting the overall health outcome.
Virtual care becomes more complicated: Providers are, by and large, not able to bill payers for additional tests, get reimbursed for hospital outpatient department fees, suggest follow-up care, or code for higher-severity conditions when working virtually. As a result, according to Gartner [2], providers with significant fee-for-service reimbursements have seen their revenue per patient visit decline when conducted virtually while continuing to shoulder the costs of facilities intended for in-person visits.
Patient outcomes don’t matter as much: There’s very little differentiation in terms of healthcare and patient outcomes because providers are only reimbursed based on a service provided and not at all over the quality of care the patient received. Doctors get paid whether or not the patient sees significant changes to their condition.
Payment is tied directly to services provided: Additionally, the fee-for-service healthcare model can actively incentivize providing unnecessary care to patients which means the patients’ underlying issues aren’t addressed. This can cause a patient to have to schedule several repeat visits due to declining health leading to more money for a practice because they can prescribe more medication and run more tests.
Technology best suited for fee for service
The fact that fee for service is so entrenched in the healthcare industry can be considered another pro because it means that the system is familiar to everyone, and both information and technology, such as medical billing software, are readily available to help practices implement and navigate it.
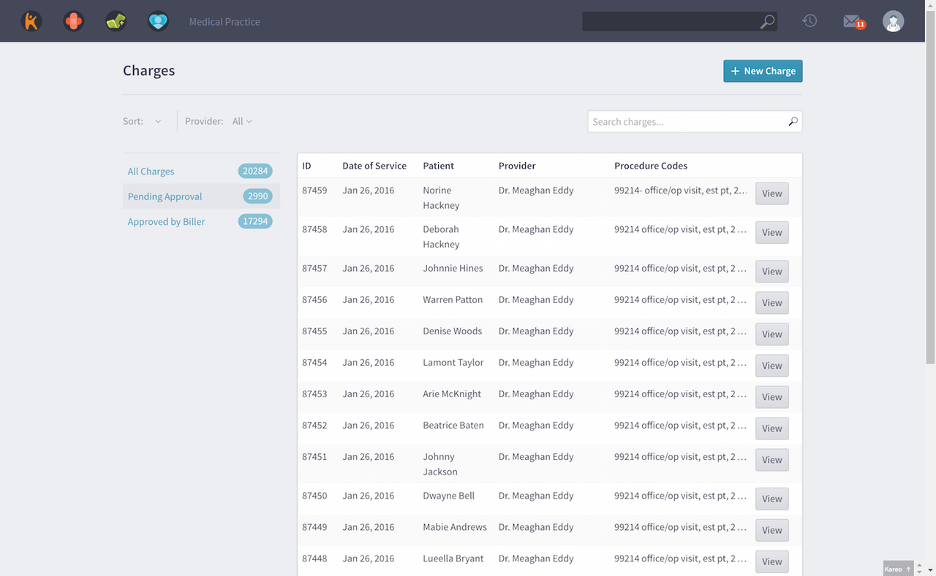
Kareo Billing’s list of charges view (Source)
Ultimately, though, because fee for service is the dominant medical payment model, you shouldn’t have any problem finding technology built with it in mind.
Fee for service is best for you if…
Adopting a fee-for-service model is right for you if you want to benefit from the years of institutionalized knowledge and infrastructure that’s been built up. You don’t need to worry about educating patients because they have an implicit understanding of how the system works. After all, a fee-for-service model is just what they’re used to, and most patients expect that.
Better software integrations, easier billing and coding, and a wider patient base are all legitimate reasons to consider fee for service as your payment model.
Concierge medicine gives group and solo practices more control over their practice
Concierge medicine is a membership-based practice model that provides patients with more access to their healthcare provider. Patients pay a monthly or yearly subscription fee ranging from a few hundred dollars a month to thousands of dollars a month, but in turn get greater and faster access to their concierge doctor.
Concierge medicine physicians can charge health insurance companies for patient visits in addition to charging the membership fees which means that healthcare organizations which subscribe to this payment model will have two forms of revenue.
The benefit of being able to charge health insurance companies in addition to the subscription fee is that it allows a concierge practice to more confidently help patients with specialty services, such as an oncology appointment, that aren’t offered by direct primary care practices.
Pros and cons of concierge medicine
Pros:
You see fewer patients: Under a more traditional primary care model, such as fee for service, doctors might see 30 to 50 patients a day, which means patients only get a few minutes with their doctor. A concierge medical practice might only see four to six patients a day, and those patients can often make same-day appointments.
Terry Bauer [1]
CEO of Specialdocs
You have a leaner staff: Without the need to worry about coding and billing, you can hire less staff which will increase your profits.
Insurance is out of the picture for the most part: You don’t have to worry about dealing with insurance companies which might also eliminate another salary you would otherwise have to pay.
Less paperwork overall: In general, there’s less paperwork involved with a concierge practice, and you won’t need to spend as much time updating your electronic health records (EHR).
Revenue streams are known and constant: You have more dependable revenue because you’re receiving consistent payments through membership fees.
You can provide the type of service you want to provide: Without having to worry about billing, coding, and insurance, you are unfettered when it comes to the types of service you can provide your patients. You can tailor your practice specifically to the needs of your patients and community.
Terry Bauer
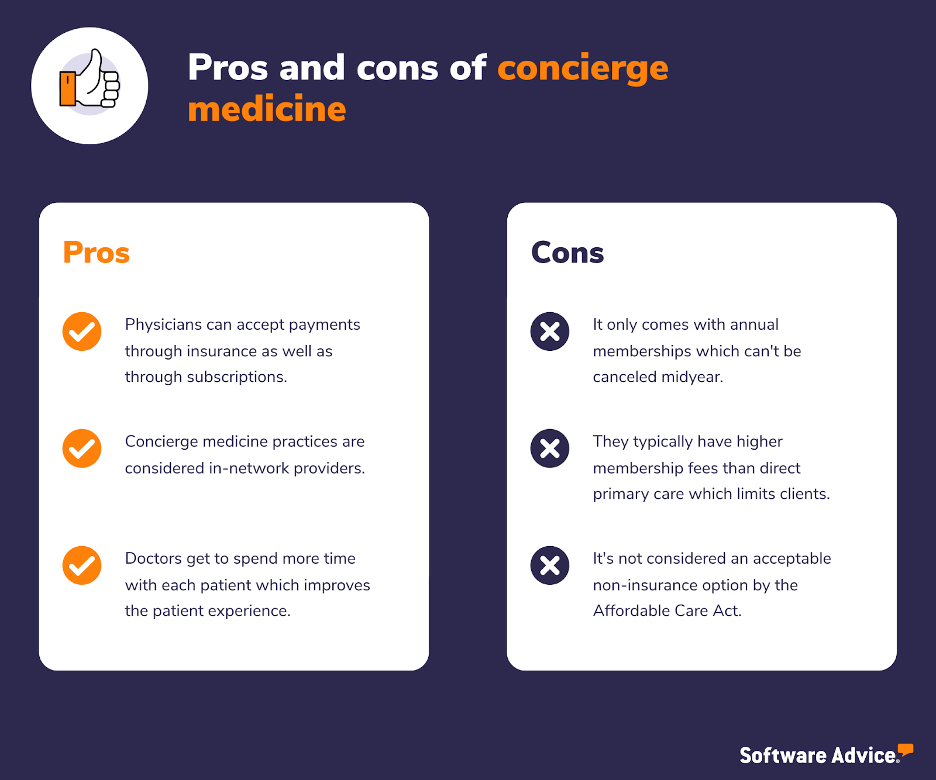
Cons:
You might lose patients: Switching to concierge medicine will inevitably cause you to lose patients since not all patients want to break away from traditional healthcare. Additionally, some patients might not make the cutoff for your new patient book.
Patients will expect more hands-on care: Because patients are paying a subscription directly to your practice, they will have higher expectations for the level of care they receive. Your patients will inevitably be more in tune with their health needs, which means they will be more hands on when it comes to their healthcare.
Your hours might be more sporadic: Concierge medicine comes with perks for your patients such as direct access to you for questions and concerns. This can sometimes happen 24 hours a day, which might mean you’re having to provide care at uncertain times. You can always specify specific boundaries, but you might lose patients to other practices who offer more comprehensive services.
Pricing structures are complicated: Finding the right balance between profitability and affordability for patients can be difficult. Setting a price that is enticing to patients while still making your practice enough money to profit and operate is difficult. A quick way to get an idea about what the right price might be is to look at other concierge practices in your area and how they price their services.
What technology is best for concierge medicine?
Patient portal software is a versatile solution that provides users with secure access to medical records and services. It boosts patient engagement by facilitating tasks such as scheduling appointments, requesting prescription refills, and making online bill payments.
Concierge practices might be interested in the ability to exchange messages with patients through the portal instead of over the phone. Most systems provide a secure electronic messaging platform that emails patients when their care team sends a new message. Providers can also respond to messages that patients send through the portal.
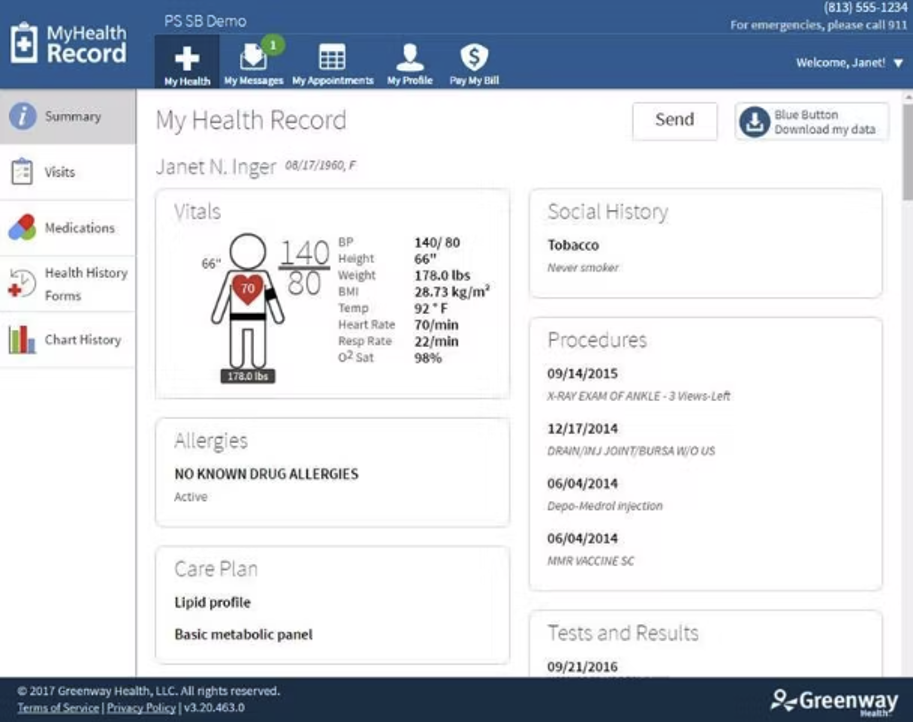
Prime Suite Software’s patient portal (Source)
The value of concierge medicine from the patient’s perspective is that they get to feel a greater level of accessibility to, and attention from, their doctor. Patient portals provide a platform on which doctors and patients can securely exchange messages, schedule appointments, and review medical notes any time of day.
Interested in figuring out ways to get your patients to use your patient portals? Check out How To Increase Patient Portal Use by Educating Patients.
Concierge medicine is best for you if…
If you’re thinking about starting your own practice and are unsure if concierge medicine is right for you, consider the following questions:
Are you often frustrated by how bureaucratic the healthcare system has become?
Do you still want to offer some specialty services such as blood testing?
Do you find dealing with billing and insurance companies to be the main stressor with your professional life?
Is your favorite part of being a physician helping and building connections with your patients?
Are you a general practitioner or family physician?
If you answered yes to any of these questions, it might be worth considering a concierge medicine practice model.
Keep in mind that if you’re a specialist, concierge medicine likely isn’t going to be a good fit for you because those services aren’t typically covered or sought after. Most patients who are looking for concierge medicine are looking for general practitioners because of the nature of services provided.
Additionally, if you already have a medical practice and are thinking about making a switch, consider your patient population. Concierge medicine is typically best for patients with chronic conditions who require multiple visits to the doctor a month who can benefit from a better patient experience. Patients who are generally older with a high-deductible healthcare plan are a great fit for concierge medicine.
Direct primary care let’s you provide the most personalized care
Direct primary care is a membership-based payment and practice model where patients are charged a yearly or monthly fee to gain access to a doctor instead of going through health insurance.
Much like concierge medicine, direct primary medical care is centered around providing a better patient experience while giving healthcare organizations consistent revenue without forcing them to spend time coding and billing.
Unlike concierge medicine, direct primary care practices do not accept any insurance whatsoever, which means patients who do not have insurance or do not want insurance are much more likely to subscribe to a direct primary care physician.
Additionally, unlike concierge medicine, patients aren’t locked into year-long contracts and can opt into monthly contracts instead of yearly contracts which gives them more flexibility and autonomy.
The Affordable Care Act explicitly states [3] that direct primary care (DPC) is a suitable non-insurance option for patients while concierge medicine is not, which means your patients won’t be charged any state-mandated fees for being uninsured as long as they pay into your practice model.
Patients who are seeking direct primary medical care are those who are looking for a personalized physician experience for a more affordable price compared to concierge medicine or traditional fee-for-service payment models. A typical direct primary care patient might be someone without any serious medical conditions who enjoys having greater access to their doctor.
Additionally, patients might seek out DPC because they want more one-on-one time with their physician.
According to our Software Advice 2022 Patient Experience survey**, over one-third of patients polled say they spent 10 minutes or fewer with their provider during their appointment, and nearly half only received between 10 and 20 minutes of care.
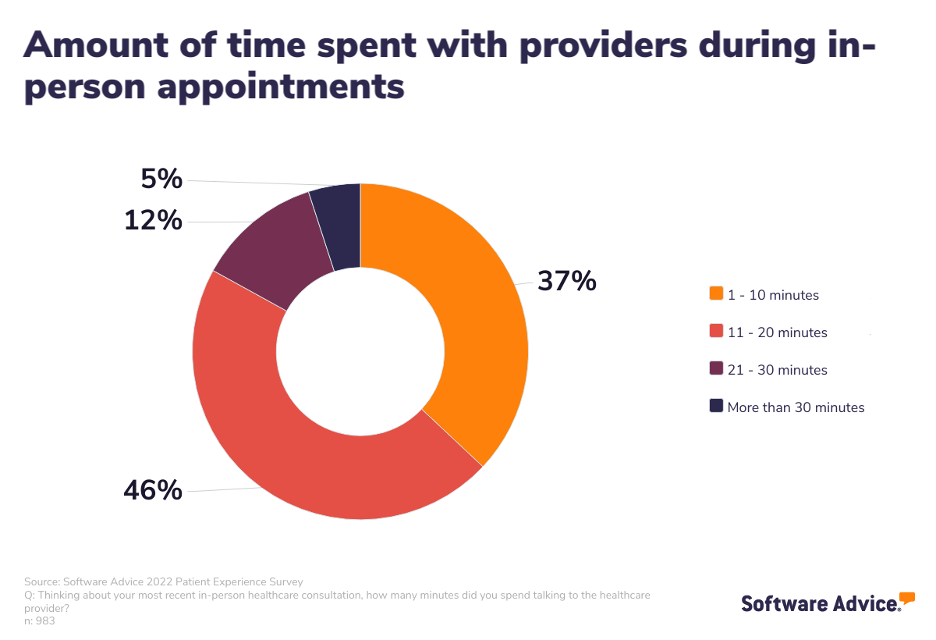
This data becomes even more compelling when you consider that most patients are forced to take between one and three hours off work in order to attend in-person medical appointments. At most, patients are only seeing doctors for one-fifth of the time they take off work to do so, the consequences of which include:
Patients don’t feel their time is valued by healthcare providers
Patients will not see the time and effort as worthwhile from a financial standpoint
Patients can seek other providers or put off care entirely**
Pros and cons of direct primary care
Pros:
Doctors and patients have more flexibility: In general, you have much more flexibility in determining what approaches and services are best for your patients because you aren’t worrying about coding and billing each service you provide.
Patients are more invested: The process between patient and doctor tends to be much more collaborative because the patient is more invested in their health outcomes.
The doctor-patient relationship is stronger: Because you have a smaller number of patients, you are able to get to know each of them better while simultaneously spending more time with each to gain greater insights into their health and needs.
Insurance isn’t a hassle: You don’t need to deal with insurance paperwork or reporting. Enough said.
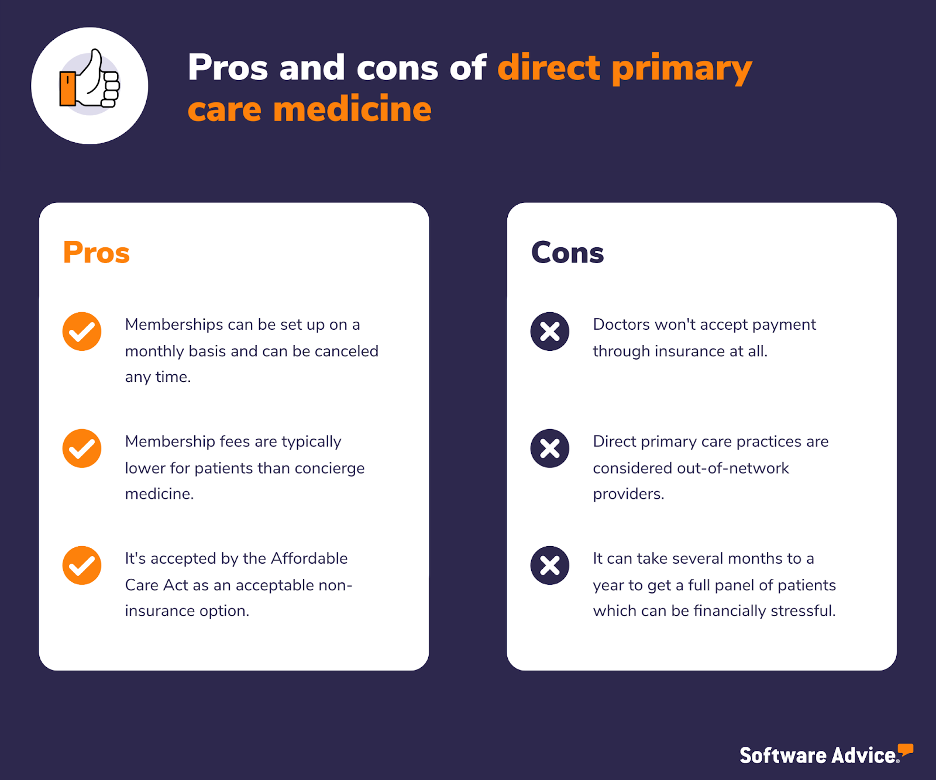
Cons:
You might lose patients: Much like with concierge medicine, you’re going to lose patients if you switch from a more traditional model.
Insurance is 100% out of the picture: You cannot accept payment through insurance at all. While also a benefit due to the lack of worrying about coding and billing, it can severely limit your ability to attract new patients.
It’s more expensive for your patients: Your patients will still likely need insurance for specialty and other types of care which means the healthcare cost is greater overall for your patients.
Patients are harder to find: On that note, it can often take months or even years to get a full panel of patients.
What technology is best for direct primary care?
DPC practices can benefit more from patient scheduling software than other types of medical practices. The nature of DPC means that your patients, in general, have greater access to you and can schedule appointments anytime they want, oftentimes same-day appointments.
That’s why providing patients with access to a tool that allows them to self-schedule is invaluable. With patient scheduling software, your patients can log in and look at your open availability and schedule something as soon as is convenient for them.
The software will then alert you of a new patient appointment.

NueMD’s scheduling software (Source)
While generally useful for all types of medical practices, scheduling software’s full potential is unlocked in a DPC practice.
Direct primary care is best for you if…
The considerations about starting a direct primary care practice are very similar to those of starting a concierge medicine practice, but with a few key differences:
Because you won’t be accepting insurance, such as Medicare or Medicaid, do you want to treat typically younger, middle-income patients?
Are you often frustrated by how bureaucratic the healthcare system has become?
Do you find dealing with billing and insurance companies to be the main stressor on your professional life?
Is your favorite part of being a physician helping patients and building connections with your patients?
Are you a general practitioner?
If you’re tired of dealing with administrative tasks, such as coding and billing, or want to build stronger relationships with your patients, you should consider direct primary care as a payment model if you’re starting your own practice. Direct primary care practices do not need to maintain staff dedicated to organizing, reviewing, filing, and managing payment claims to third-party payers.
A practice who is thinking about making the switch to direct primary healthcare should poll their physicians to see if they align with the new direction. Ask the above questions to determine if they are interested in spending more time with their patients while also seeing less patients on average.
Poll your patients about their interest in the new payment model. The reality is that if you do make the switch to direct primary health care, you’re going to lose patients, but what you gain is a patient population who is more dedicated to your practice.
Value-based care puts the emphasis on patient health outcomes over anything else
Value-based healthcare is a pricing model that incentivizes your practice based on the quality of services you provide to patients. Within a value-based payment model, your practice is compensated depending on a patient’s health outcomes.
The goal of a value-based care system is four-fold:
Improve the quality of healthcare
Improve the patient experience
Lower costs for patients
Improve the care team’s experience
Healthcare providers need to produce data to demonstrate clinical outcomes that measure these four metrics in order to show improved health outcomes for patients. To do that, doctors must leverage modern data by using software to support decision making when transitioning to a value-based care model [4].
Pros and cons of value-based care
Pros:
Patients get more bang for their buck: Patients spend less money for better healthcare because value-based care doesn’t incentivize practitioners for throwing solutions at the wall to see if they stick. That means providers won’t benefit from recommending services their patients may not need or treatments that may not work, which will save patients money.
Patient experience and engagement are prioritized: Providers are equipped to offer a better patient experience because a value-based model requires them to be more efficient and strategic with the care delivery they offer during each patient visit. It rewards you for delving deeper into the underlying problems your patients may be experiencing instead of just running several tests, which can be costly, stressful, and uncomfortable for patients.
The doctor-patient experience is less transactional and more personal: During initial consultations, doctors and nurses spend time with their patients to get a more holistic idea about the reason for their visit. This improves the healthcare experience for patients, as their needs are personally attended to.
Patients receive true value with their healthcare spending: Traditional payment models incentivize doctor visits and prescriptions at their current prices, leading to inflated healthcare costs. Because of the high costs of more traditional medical payment models, many patients choose not to address their health issues until it’s too late or things have grown out of control, which becomes more costly in the long run. With value-based care, patients feel like they’re getting their money’s worth.
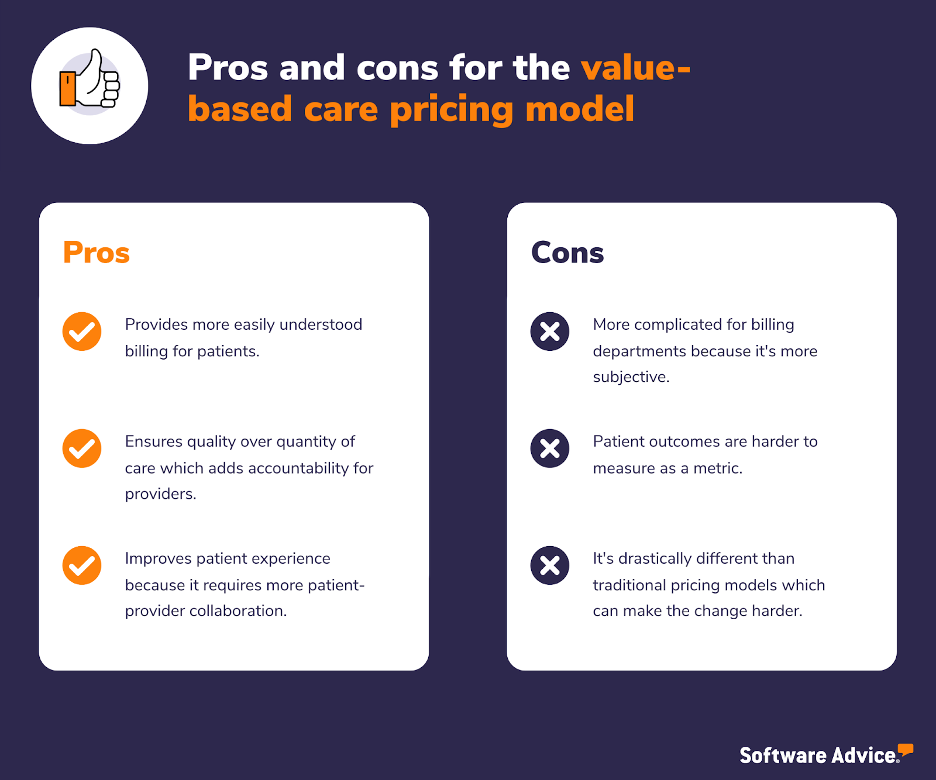
Cons:
More regulations and tracking occur: Although value-based health care is typically more beneficial for patients, it can be a hassle for practices because of the increased regulations placed on a healthcare provider. Because the government sets the terms of value-based care, it restricts how much you and your practice can do.
It’s hard to make the shift to value-based care: Because fee for service is so entrenched in the healthcare industry, it can be a tough sell for an entire healthcare organization to make the shift because of the uncertainty that comes with it.
Tech can be harder to find: Technology and infrastructure are still largely focused on accommodating that pricing model. You might also struggle to get buy-in from your staff and stakeholders because of the initial cost of making the shift from fee for service to value-based health care.
Tracking metrics is more complicated and subjective: Because billing is tied directly to the quality of patient care delivery, a provider needs to invest heavily in resources and software tools that are necessary to track important health metrics such as hospital readmissions, adverse events, population health, and patient engagement during treatment.
Here's a quick video we created that goes over the pros and cons of value based care:
What technology is best for value-based care?
A robust patient experience and engagement suite of software is beneficial to a value-based care practice because so much of your revenue is tied to patient outcomes, and more engaged patients are more likely to stick to their health plans.
We’ve written a lot about how practices can increase patient engagement and how technology can specifically help with patient engagement strategies, so for more information and resources, check these other blog articles out:
Value-based care is best for you if…
Value-based care is very likely the future of healthcare. Fee for service is unquestionably the most widely-used reimbursement method at the moment, but that won’t always be the case.
The benefits to your patients might be enough incentive, but you might also want to make the switch to this payment model if you want to be ahead of the competition as more and more healthcare organizations switch.
In fact, more healthcare regulations are being rolled out each year to incentivize the switch to value-based care [5] because it’s cheaper for patients and insurance organizations.
Additionally, insurance companies don’t have to pay as much for patient readmissions which means they are making more money, and patients are healthier and more equipped to manage their conditions.
The Affordable Care Act requires an annual, minimum 80% Medical Loss Ratio (MLR) [6] for individual and small group insurance plans, and an annual, minimum 85% MLR for large group plans. Congress imposed the MLR to provide greater transparency and accountability around the expenditures made by health insurers and to help bring down the cost of healthcare.
In addition to the ACA requirement, the Centers for Medicaid and Medicare Services (CMS) [7] is looking to push healthcare in the U.S. toward total adoption of value-based care by 2030 which means more insurers are jumping on board early and adopting value-based care reimbursement.
Aside from generally wanting to provide the best care for your patients as possible, the shift toward value-based healthcare is coming, so the sooner you and your practice hop on board, the better suited you are going to be to handle the organizational changes made by CMS and insurers.
Other types of payment models you might see
The above are some of the more common types of payment models you can find and are by no means a comprehensive list. In addition to the aforementioned, you might also see an alternative payment model option:
Bundled payment: In a bundled payment model, practices receive payment based on episodes of care. An episode is a set of diagnoses and services provided over a specified period of time, most typically used for surgical procedures.
Bundled payment bundles hospital, physician, and post-acute healthcare services together and allows practices to achieve higher revenue by avoiding complications, negotiating discounts, and choosing lower-cost settings for post-acute healthcare.
Capitation: In a capitation payment model, practices receive payment to manage a patient’s care and health conditions per patient per period. Most periods are one month, and the health plan will apply attribution rules to decide which patients are included in a given physician practice.
There are also several supplementary payment models such as pay-for-performance, shared savings programs, or retainer-based payment plans which all come with their own lists of pros and cons.
The decision is up to you, but we’re here to help
Ultimately, it’s up to you to determine what payment model is best for your practice, but we’re here to help you narrow down your choices in order to make the best decision possible. Once you’ve factored in all of the different pros and cons that go into determining which healthcare payment model you want to pursue, it’s time to start thinking about which software is most beneficial to your new practice.
That’s where our software advisors come in. At Software Advice, we guide you to the right software with real advice from real people—our advisors have helped hundreds of professionals in your industry. We’re here to help you find solutions that meet your needs and budget.
You can chat online now with an advisor or schedule a phone call. In just a few minutes, your advisor will help you narrow down a list of options that meet your needs.
Sources
Terry Bauer, LinkedIn
Affordable Care Act, Healthcare.gov
HDO CIOs Must Fully Leverage Key Data Sources to Succeed in Value-Based Care, Gartner
CMS Medicare Access and CHIP Reauthorization Act (MACRA), Centers for Medicare and Medicaid Services
Medical Loss Ratio Requirements Under the Patient Protection and Affordable Care Act (ACA): Issues for Congress, Congressional Research Service
Innovation Strategy Refresh, Centers for Medicare and Medicaid Services
Survey methodology
* Software Advice’s 2023 Medical Chatbot Survey was conducted online in January 2023 among 65 respondents in the U.S. Respondents were all medical providers, practice owners, and administrative staff who are currently using a chatbot to field inquiries from patients at their practice.
** Software Advice's 2022 Patient Experience Survey was conducted online in October 2022 among 1,001 respondents in the U.S. Respondents were all adults who had visited a healthcare provider within the past three years.