Guide to Medication Compliance in Mental Health Patients
“I woke up medicated, in four-point restraints, in the quiet room of a private psychiatric hospital in 1995. . .”
So begins Eric Arauz’s personal account of a years-long struggle to accept his psychiatric medication regimen. Today, he’s a successful author and mental health care advocate working to improve the way patients and providers approach the subject of medication compliance.
We interviewed Arauz and conducted our own primary research to show mental health care teams how patients can be encouraged to take medications as prescribed.
This guide also explores new and existing technologies, outreach tips and communication strategies you can apply at your practice today.
Here’s what we’ll cover:
The Importance of Medication Compliance in Mental Health
Patient Survey: Top Reasons for Noncompliance
5 Best Practices for Noncompliance Intervention
New Technologies for Improved Medication Compliance
The Importance of Medication Compliance in Mental Health
In Gartner’s Hype Cycle for Consumer Engagement With Healthcare and Wellness, 2016 (available for Gartner clients), the authors describe why medication compliance is such an important issue:
“An astonishing number of patients (sometimes reported at 80 percent and rarely, if ever, below 30 percent) do not take or use their prescribed medicines as recommended by their prescribers. This results in suboptimal health outcomes, wasted expenditures on medications and excess hospitalizations.”
Jeff Cribbs and Richard Gibson, M.D.
Arauz points out that medication adherence is a challenge for patients with any illness—not just mental health disorders.
However, Gartner’s analysts say it’s particularly important for people with behavioral disorders and chronic conditions to practice medication compliance because noncompliance can lead to “worsening clinical status, emergency department visits and hospitalization.”
Psychiatric patients can experience these consequences even if they’ve only missed a couple of doses. For this reason, mental health care professionals should routinely check in with patients about their adherence rates.
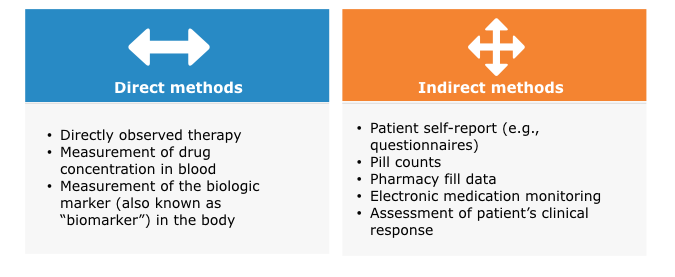
Researchers say this can be done through direct or indirect methods, including the following:
Methods of Measuring Medication Adherence
Patient Survey: Top Reasons for Noncompliance
To understand why some people don’t adhere to their prescribed drug regimen, we surveyed 205 psychiatric patients who have been in treatment for at least six months.
We asked them which of the following reasons describe why they’ve deviated from their prescription medication schedule. Respondents selected all answer options that applied to them.
Top Reasons for Medication Nonadherence in Psychiatric Patients
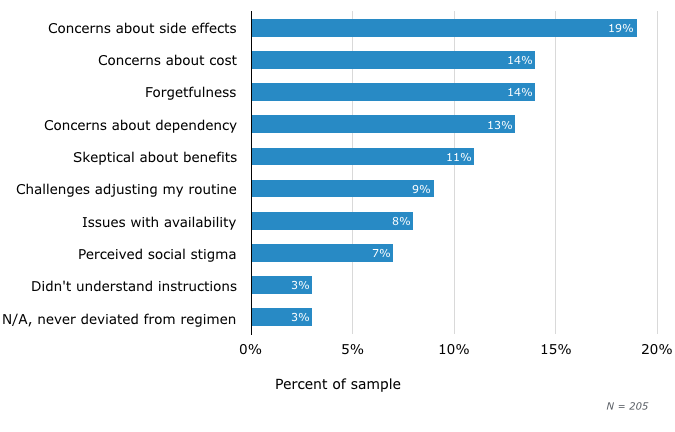
The greatest percentage of people say side effect concerns keep them from taking mental health medications as prescribed. Arauz has experienced such side effects first hand and says they can be particularly tough to handle when a new medication is incorporated into the patient’s care plan:

“It might take anywhere from two to eight weeks for a patient’s medication to start being efficacious, so now they’re feeling both their [original] symptoms and the medication’s negative side effects. It’s a very disorienting journey.”
Eric Arauz, author and mental health care advocate
He says patients dealing with side effects may find it helpful to evaluate medications in 30-day, 90-day and one-year periods instead of focusing on how they’re feeling on a particular day. That way, it’s easier to see long-term progress and withstand discomfort or pain.
The second most-cited reason for nonadherence is concerns about medication costs. Fourteen percent of respondents struggle with this factor, which is worrisome but not surprising due to the health care industry’s steadily increasing drug costs.
If one of your patients is in this situation, consider sharing this helpful resource list from Mental Health America. It tells patients how they can get help paying for prescriptions through nonprofit and government programs.
Finally, the third reason patients cited for missing medications is forgetfulness. Slips and lapses are common even for patients who are motivated to follow a treatment regimen. Skip down to the section of this article titled “New Technologies for Improved Medication Compliance” to discover innovative ways of addressing this roadblock to adherence.
5 Best Practices for Noncompliance Intervention
So now that we know why some patients struggle with adherence, what can we do about it? Here are five best practices that mental health professionals should incorporate into their medication noncompliance intervention strategies:
1. Practice empathy
Arauz says coming to terms with a psychiatric diagnosis can feel like “an absolute atom bomb for a lot of people” because it impacts their sense of self. Most of their defining characteristics: the way they behave, how they perceive and react to the world—these cognitive functions will likely be affected by medication, but it’s difficult to predict how or when. That’s a very vulnerable position to be in.
For this reason, it’s important for mental health professionals to practice empathy in all of their patient interactions. While this may seem like an obvious recommendation, it cannot be overstated, and many industry leaders agree there should be more professional training on this topic.
2. Find out the patient’s attitude toward medication
It stands to reason that patients’ opinions on medication will influence their desire to take it. Therefore, it’s important to evaluate whether someone has preconceived notions, fears, goals and/or hopes regarding a particular drug.
A good way to gauge these feelings is by performing the Drug Attitude Inventory assessment or using the questions in it as a basis to guide discussions with patients. This can be done before a new medication regimen begins and while it’s underway (e.g., every quarter or annually).
For practices using electronic medical records software, it can be especially helpful to record the results of a Drug Attitude Inventory assessment over time and see if trends emerge.
3. Employ a shared decision-making (SDM) care model
Arauz is a big proponent of this model because “it gets the patient more ‘bought into’ what they’re working toward.” Indeed, studies have shown a positive relationship between patient participation in decision-making and treatment adherence in the mental health care field.
Here are some ways you can apply SDM principles to your practice, assuming the patient has full decisional capacity:
Encourage patients to research any recommended medications on their own (plus any alternatives they’re curious about) and then discuss the pros and cons with you.
Give patients the option to switch to a different drug or dosage if they’re having too many side effects with a particular brand.
Work together to simplify a patient’s drug regimen if it’s too complicated.
4. Show patients long-term medication adherence is a good thing
Not every patient requires a long-term relationship with prescription drugs, but those that do resent it. After all, 13 percent of our survey respondents cited a “fear of dependency” as a reason for their nonadherence.
“Some patients almost define recovery as being off medication and don’t understand why they’re still on it if they haven’t had a [mental illness] symptom in 10 years,” says Arauz.
His suggestion for treating physicians is to give patients examples of successful people that have maintained long-term or lifelong medication adherence. This can serve as inspiration and redefine their idea of recovery.
5. Make treatment recommendations beyond medication
No matter how effective a medication may be at abating symptoms, it’s not the be-all and end-all of mental health recovery. Researchers recommend psychiatric patients leverage therapeutic support services, such as cognitive behavioral therapy, to create a more multifaceted approach to their well-being.
Arauz is also in favor of this kind of comprehensive care plan because factors such as the availability of a support network (e.g., friends and family), dietary habits and physical fitness can make a huge difference on the path to wellness.
“That approach even takes some of the pressure off the medication,” he says. “Identify what are the elements in a patient’s life that could act as anchors for them to find satisfaction so they don’t put all their hope on a ‘magic pill’.”
New Technologies for Improved Medication Compliance
In the Gartner Hype Cycle report we referenced earlier, the authors list existing and emerging technologies that can make medication compliance easier. Check out images and descriptions of these technologies by clicking through the slideshow below:
Medication Compliance Tools and Technology from Software Advice
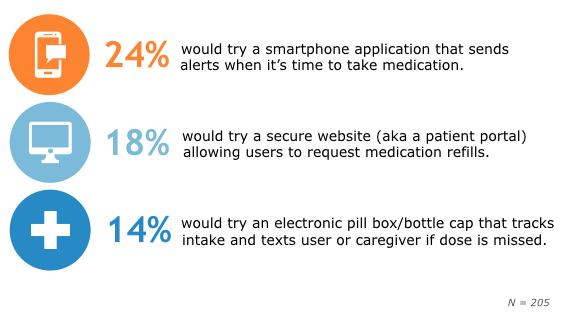
But would patients actually embrace any of these tools? We asked our survey respondents to select which of those technologies they’d choose to use for medication adherence. Here are their top three choices:
Top Technologies Patients Would Use for Medical Compliance
Most of those solutions are meant to be purchased by the patients themselves, but you can get patient portal software for your practice if you’re interested. Here’s a list of popular systems, or email me at gaby@softwareadvice.com for a recommendation within your budget.
Conclusions and Next Steps
Medication adherence is a challenge for patients in every stage of their treatment, which is why it’s good to stay on top of new ideas to curb noncompliance. Here’s a summary of our key survey findings and some best practices for you to consider:
One in five psychiatric patients surveyed (20 percent) say they’ve deviated from a medication regimen because of concerns about side effects.
To help patients withstand pain or discomfort due to side effects, practice empathy while discussing their symptoms. Also consider employing an SDM care model when adjusting their dosage or switching to an alternative prescription.
Nearly one-quarter of patients surveyed (24 percent) say they would likely use a smartphone application for medication reminders.
This is an encouraging statistic because it shows a significant amount of people are willing to use tech-based tools as a proactive measure to adhere to their regimens.
The second most popular technology among patients is a portal to request refills. This is particularly significant considering 11 percent of psychiatric patients miss doses because of availability issues.
Consider investing in patient portal software, which can either be integrated into a mental health EHR system or purchased as a stand-alone system. For more detailed information on patient portal selection, implementation and engagement, read our full report here.