New Medical Practice Checklist: How To Get Started
Jump to:
Step #1: Prepare your practice
Step #2: Organize your operations
Step #3: Buy software and supplies
Step #4: Define staff workflows
Step #5: Promote your services
Starting a new medical practice can be nerve-wracking. The rate at which large medical organizations and hospitals are buying out small, independent practices [1] represents a “tide of consolidation” that threatens the survival of existing private medical practicess and challenges the development of new practices.
This consolidation rate is projected to grow as a result of increased financial strains on the healthcare industry [1]. Knowing this, it’s more important than ever for physician entrepreneurs such as yourself to plan ahead when opening a private medical practice.
That’s why we put together a checklist for new medical offices. It combines insights from several industry associations, physician surveys, medical software tips, and an interview with startup practice expert Dr. Pamela Wible. [2]
For an easy-to-follow guide on what you need to do, simply download our checklist and read the detailed explanations below.

Note that this checklist excludes a few tasks that everyone opening a new private medical practice should complete early on, such as:
Obtaining a state medical license
Applying for a narcotic license (if necessary)
Choosing a location
Once those are done, you can start checking off items on your main list. Here are some more details and expert advice to help you with each phase.
Step #1: Prepare your practice
Let’s go through the tasks involved in getting your new practice started.
Determine the business model and entity type
The first step is to decide what type of medical practice you want to operate. Here are a few of the most common practice models to help you start thinking about your options:
Traditional | Physicians collect patient co-pays and bill insurance companies to receive reimbursement for services rendered. They see many patients to cover costs. |
Concierge (aka boutique or retainer practices) | Patients pay a flat membership fee for medical services instead of, or in addition to, billing their health insurance company. Physicians see fewer patients than usual and are, therefore, expected to be more accessible. Read more about concierge medicine here. |
Direct primary care (aka ideal medicine or direct pay practices) | Patients pay a flat membership fee for medical services, but the fee is usually lower, and insurance is never accepted. Physicians sometimes see fewer patients than usual. They may or may not make themselves more accessible to patients. |
Dr. Pamela Wible favors the direct primary care model, particularly for physicians who are choosing a solo practice as a result of bad experiences with employers in the past.
Dr. Pamela Wible
Some physicians get burned out dealing with insurance payers and complying with ever-shifting government healthcare regulations (e.g., HITECH, MACRA, and HIPAA) to meet reimbursement requirements. If that sounds like you, consider starting a concierge or direct primary care practice. These models allow you to spend more time with individual patients since there are fewer patients to treat, requiring less red tape.
However, before finalizing your decision, think about what kind of business entity is best for you. For example, do you want a sole proprietorship? A partnership with a colleague? A limited liability company (LLC)? Each of these options has its own benefits and drawbacks, so consult a lawyer to understand your choices and pick the best one.
Open a practice checking account
Once you’ve decided on your business model and entity, open a medical practice checking account at the bank, and apply for a loan if you need one. Now would be a good time to find an accountant, if you haven’t already, and consider purchasing medical accounting software.
Get a tax/employer identification number
Lastly, call the IRS to obtain a federal taxpayer identification number (TIN) or an employer identification number (EIN) for your business. Also, register for state and local taxes; learn more about them through state government sites depending on where your practice is located.
Step #2: Organize your operations
Here’s what you need to do to organize operations at your new practice:
Get malpractice insurance
Malpractice insurance is important, but it shouldn’t cost you an arm and a leg. Wible says insurers regularly provide discounts that can save you money on your premiums [3]. While you’re shopping around for medical liability insurance, ask carriers if they also offer corporate, health and disability, and/or personal life insurance coverage.
Set up a fee schedule
Another key task for organizing operations is to develop a fee schedule, which is a simple list of all the services you’ll offer and the amount you’ll charge for each. One of the best ways for medical professionals to do this is to see what other healthcare providers in their area are charging.
Ask your colleagues for a copy of their fee schedule to get some ballpark figures, then see what adjustments you should make to make ends meet. Check out the AMA [4] and CMS [5] websites for additional resources.
Get your credentials
To wrap up the planning phase, you may have to prepare a Medicare and/or Medicaid provider application.
Additionally, you must submit applications with individual insurance providers to be authorized to receive reimbursements from them. This credentialing process can take 90 days or more [6], so begin submitting applications to private health insurance companies well ahead of your business opening. (Note: Direct primary care practices and some concierge practices don’t require these additional steps.)
Regardless of who you’re applying for credentialing with, it’s wise to gather all the documents you’ll need, convert them into PDF files, and store them on your computer. That way, you’ll be able to access and share all of your important business paperwork quickly.
Step #3: Buy software and supplies
The next step is setting up the software apps and medical supplies you’ll need.
Choose electronic health records (EHR) software
Electronic health records (EHR) software will make running a medical practice much easier by safely storing patient data, automating appointment reminders and scheduling appointments, minimizing resource consumption, and improving the quality of the care you offer to patients. EHR systems, however, do take time and money to implement, so it’s best to start shopping for EHR software early on.
A good place to start would be looking at popular systems and seeing which fit the needs of your new medical practice.
Read more about selecting the most affordable option for your practice by checking out “5 Easy Steps To Pick the Ideal Free or Open Source EHR.”
Decide between billing software or outsourcing
If you want to keep all processes within your business, another health IT tool worth investing in is medical billing software, which allows you to handle coding and collections in house.
On the other hand, a dedicated billing system may not be necessary if you decide to outsource the service. Think carefully about how you’d like to handle this important component of practice management.
Check out “How Small Medical Practices Can Understand and Optimize Their Revenue Cycle” to find out more about running your own revenue cycle.
Obtain medical equipment and tools
When it comes to supplies, frugality is a good idea when your business is just getting started. “Don’t fall into the high overhead trap,” says Wible.
She explains there are various pieces of professional medical equipment you can get for free by reaching out to retiring doctors or overstocked hospitals.
Here’s a list of common necessities:
Equipment: Exam tables, stethoscopes, otoscopes, blood pressure monitors
Hardware: Fax machines, computers, phones, credit card machines
Supplies: Ointments, gloves, scalpels, syringes, gauze, antibacterial wipes, tongue depressors
Services: Utilities, phone, internet
Clothing: Lab coats, staff uniforms, name tags, patient gowns
Furnishings: Chairs, tables, decorations
Step #4: Define staff workflows
Below are the tasks for setting up the human resources (HR) department for your new private practice:
Delineate employee roles
By this point, you should be able to tell how many staff members you’ll need to run your medical practice.
For example, if you choose not to outsource billing and expect to build a large patient panel, you would benefit from a dedicated employee to handle billing and scheduling as well as a nurse or medical assistant.
Likewise, if your business depends heavily on Medicare reimbursements, you may want to bring on a compliance officer to ensure all the requirements are met and to watch for regulatory changes.
Set up personnel benefits
Your next step is to define the expectations for each role before the hiring process begins. Also, create an employee handbook that reiterates those expectations.
In the handbook, include your medical office policies (e.g., time and attendance) and benefits (e.g., health insurance options and paid time off). Take the time to set up these benefits and arrange for payroll services, if needed.
Perform a security risk assessment
As you figure out staff workflows, you’ll also have to address patient privacy and security issues. To comply with HIPAA and MACRA, you’ll need to conduct a security risk assessment. The assessment should include documentation of the following:
An overview of all protected health information (PHI) you create, receive, or transmit
A list of all the physical and/or digital locations where PHI is stored or maintained
An assessment of current security measures at your medical practice
A rundown of the possible threats and vulnerabilities to PHI
An evaluation of each threat’s likelihood
A determination of the impact of potential threats
Data breaches for medical practices are common, and most of them are a result of human error. Make sure you’re training your staff on the best practices to avoid expensive HIPAA violations. Also, verify that your EHR system includes certain security features to provide additional protection.
Finally, don’t forget to create a HIPAA notice of privacy practices (NPP) for patients to sign when they fill out their registration and medical history forms.
Read “How to Strengthen Your Healthcare Data Security with Software” for more information on how software can help beef up security at your medical practice.
Step #5: Promote your services
The final step to setting up a successful practice is promoting your services and gaining visibility in the market.
Network with colleagues
Once all the logistics are handled, it’s time to start promoting your medical practice to attract patients. One of the best things you can do is network with colleagues by joining a medical association or signing up for a physician-only social network.
You’ll be able to meet specialists in your area who can refer their existing patients to your medical practice. You can also get valuable advice from peers about how they promote their practice.
“Make sure you ask for help from a trusted mentor who has already launched a successful medical clinic,” says Wible. “Too many doctors don’t ask for help and try to do this on their own.”
Build an online presence
When marketing your medical practice, it’s important to establish an online presence as soon as possible. In the Master Patient Experience Survey[*], at least 65% of U.S. patients report using online reviews as a first step to choosing a doctor.
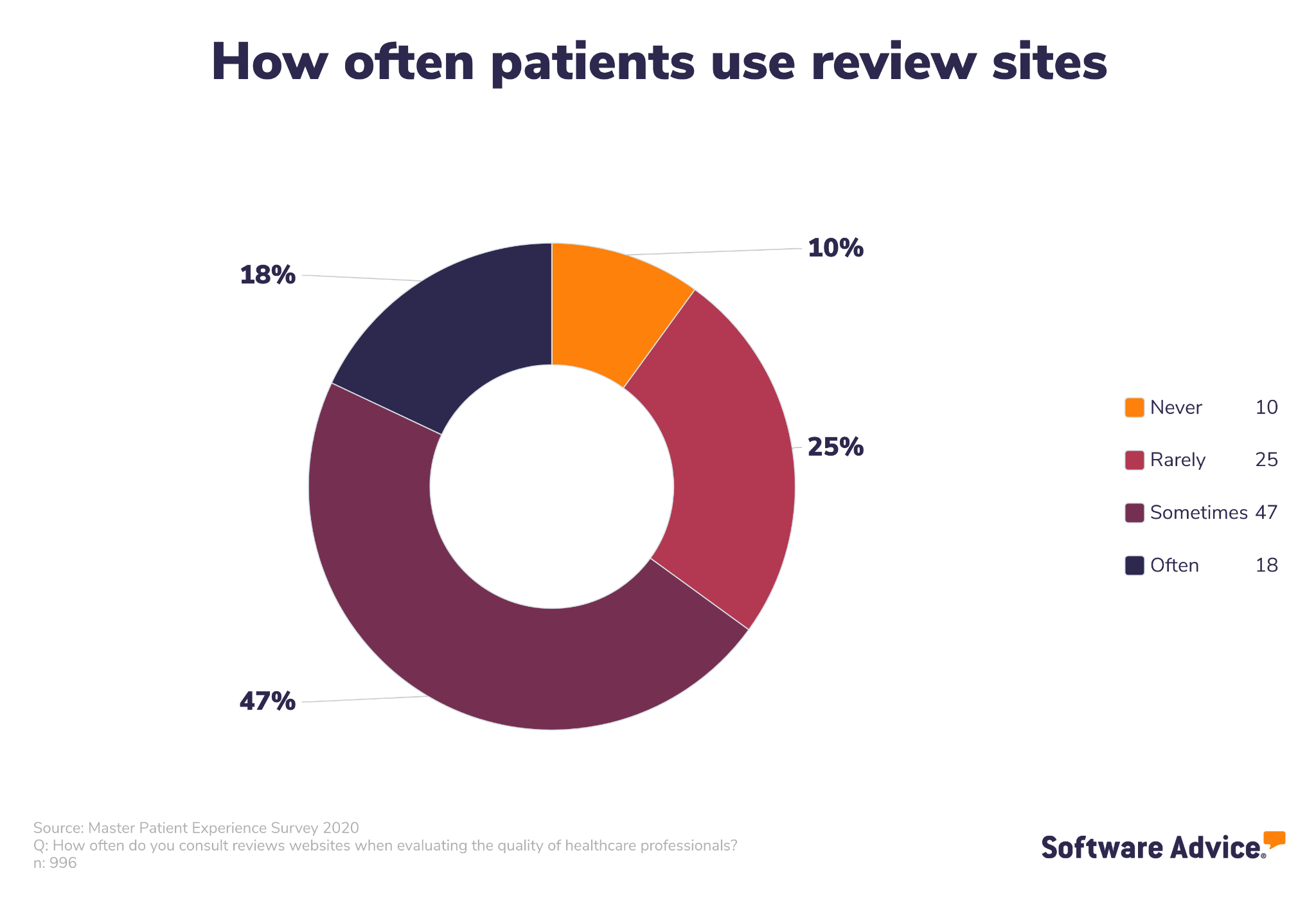
Set up a profile on platforms, such as Healthgrades, Vitals, and Facebook, so it’s easy for patients to find you. Once you start building a patient panel, encourage your patients to leave a review on one of these sites.
Create a community of patient engagement
Another good strategy is to get involved with the local community. That will help you establish personal connections with potential patients and get your practice’s name out there.
Consider volunteering, giving a speech at community gatherings (e.g., the local chamber of commerce, church groups), or hosting a health fair at a nearby park.
Don’t forget about telehealth
Many healthcare providers started to offer telehealth services to patients during the pandemic, and patients may expect these remote services to stick around: 91% of patients say they’re more likely to go with a doctor who has a telemedicine option over one who doesn’t[**].
In the early stages of opening your new practice, consider how your office will handle telemedicine, the types of telemedicine your practice will offer, and the software you might need.
Lastly, our medical practice checklist will help you open a thriving practice you’ll love working in. It may be intimidating to strike out on your own and start a new business, but the freedom you’ll feel once you’re up and running can make all the work worthwhile.
And don’t forget, once you’re ready to compare medical software options, our team of advisors is always ready to help you find products that meet your unique needs.
Schedule a call or click here to chat with a medical software advisor now to discuss your practice’s needs. Our advisors will consider your budget and feature requirements as they build a shortlist of products that fit those specifications.
Survey methodology
* Master Patient Experience Survey 2020: We surveyed over 1,000 patients in the United States. We used screening questions to narrow the number of respondents down to 990 with relevant histories and experiences. We worded the questions to ensure that each respondent fully understood their meaning and the topic at hand.
** Software Advice conducted the 2022 State of Telemedicine Survey in August, 2022 of 1,002 respondents to learn more about telemedicine use and how it has been affected by the pandemic. Screening questions were used to narrow respondents to those with relevant experience with the subject matter.
Sources
Few healthcare mergers seen so far in 2022, Chief Healthcare Executive
Pamela Wible, LinkedIn
7 Tips to Save Costs on Malpractice Insurance for Lawyers, Aon Attorneys Advantage
7 Simple Steps for Physician Credentialing, Compliance Line