Value-Based Care vs Fee-for-Service: The Ins and Outs You Need to Know
The fee-for-service pricing model has dominated the healthcare landscape for decades because of how easy it is for doctors and healthcare organizations to track billing and make money. However, more and more incentives are being passed by the Centers for Medicare and Medicaid Services (CMS) to make the switch to a value-based care pricing model with even more on the way in the coming years.
As a smaller practice, it might be hard to know when the right time to make that switch is. If you wait too long, you risk losing patients due to other practices and healthcare organizations offering the more patient-focused healthcare that value-based care incentivizes. This will lead to a loss of revenue and, potentially, an inability to recover.
That’s why small to midsize practice owners should decide if they should shift their practice toward a value-based care model instead of a more traditional fee-for-service model of healthcare. If that’s you, you’ve come to the right place.
What we’ll cover:
What is the fee-for-service care model?
In the fee-for-service model, doctors and healthcare organizations get paid based on the individual care services they provide without a focus on if that care is effective. It’s the most traditional pricing model used in healthcare because it’s easy to quantify metrics for billing purposes which makes getting paid for services much easier.
Using the fee-for-service model, a healthcare provider charges based on individual services such as appointments, treatments, tests ordered, and prescriptions given, then lists all of these services separately on a bill which can often be long and confusing for the patient.
Here’s a quick video we created that goes over the pros and cons of value based care:
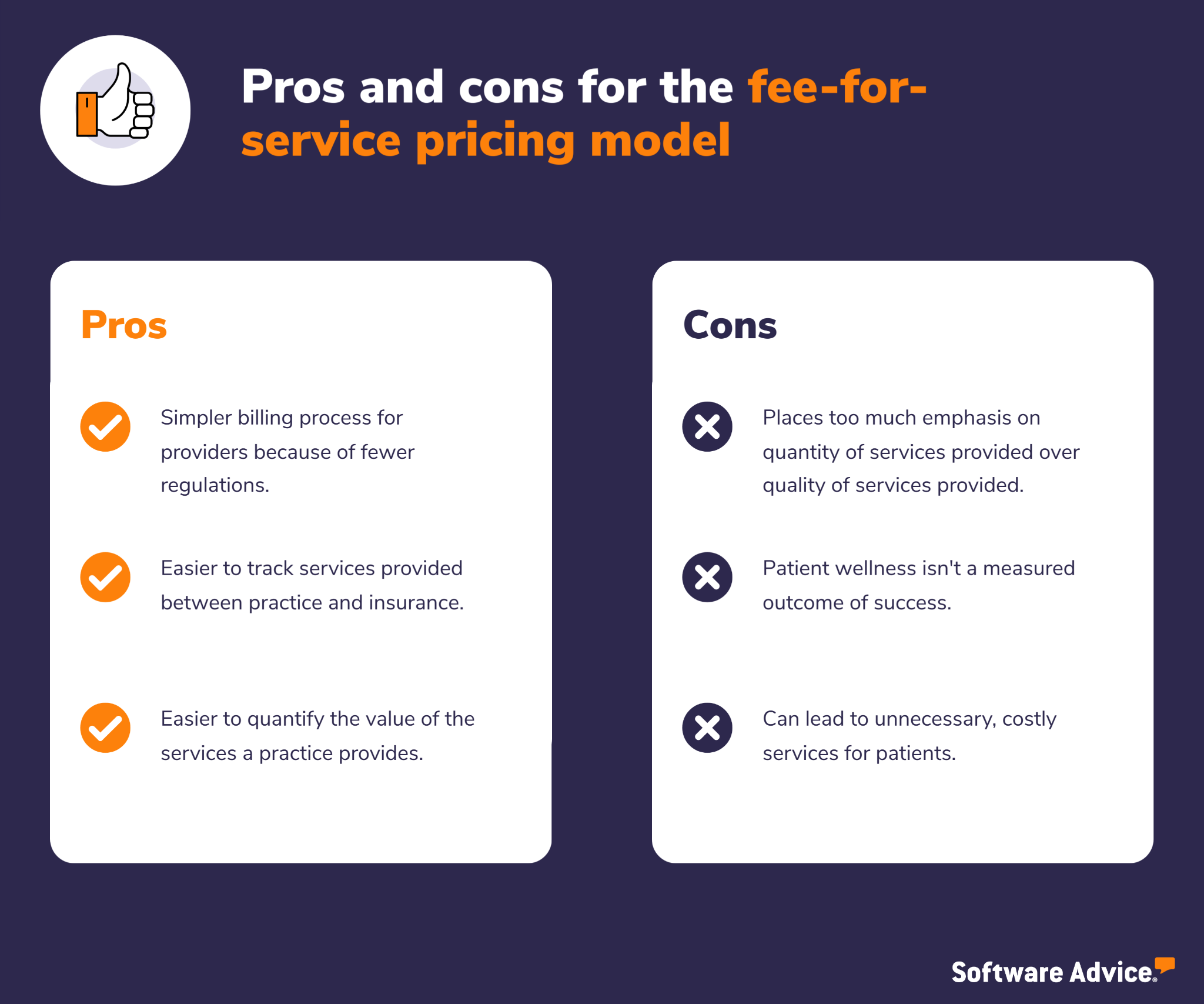
Pros of the fee-for-service healthcare model
Most of the pros of the fee-for-service healthcare model revolve around making billing easier for healthcare providers because of the straightforward nature by which they receive their payments. Additionally, for basic services, fee-for-service is a relatively simple and straightforward method for patients because the billing process for doctors and administrators isn’t complicated.
Metrics are also often easier to track because you can easily quantify the number of services you are providing and know how much each of those services cost. It makes the billing process significantly easier to track as well.
The fact that fee-for-service is so entrenched in the healthcare industry is also a positive because it means that the system is familiar to everyone and information and technology like medical billing software are readily available to help practices implement and navigate it.
Cons of the fee-for-service healthcare model
Because this model cares more about quantity of services provided over quality, it incentivizes a provider to take on as many patients as they possibly can in order to make the most money. This could mean less patient satisfaction.
Physicians spend less one-on-one time with the patients and prescribe more tests without getting to the root of what patients may be experiencing, thus impacting the overall health outcome.
There’s very little differentiation in terms of healthcare and patient outcomes because providers are only reimbursed based on a service provided and not at all over the quality of care the patient received. Doctors get paid whether or not the patient sees significant changes to their condition.
Additionally, the fee-for-service healthcare model can actively incentivize providing unnecessary care to patients which means the patients’ underlying issues aren’t addressed. This can cause a patient to have to schedule several repeat visits due to declining health leading to more money for a practice because they can prescribe more medication and run more tests.
Overall, a fee-for-service pricing model is more costly for patients because when the only condition for payment is the quantity of services provided, there’s no incentive for a provider to make operational improvements to their practice or offer higher-quality care which can lead to complacency.
What is the value-based care model?
Value-based healthcare is a pricing model that incentivizes your practice based on the quality of services you provide to patients. Within a value-based care model, your practice is compensated depending on a patient’s health outcomes.
Value-based care puts more emphasis on ensuring healthcare providers like you take care of patients’ medical needs in as few visits as possible and to the best of the physician’s ability.
The goal of a value-based care system is four-fold:
Improve the quality of healthcare
Improve the patient experience
Lower costs for patients
Improve the care team’s experience
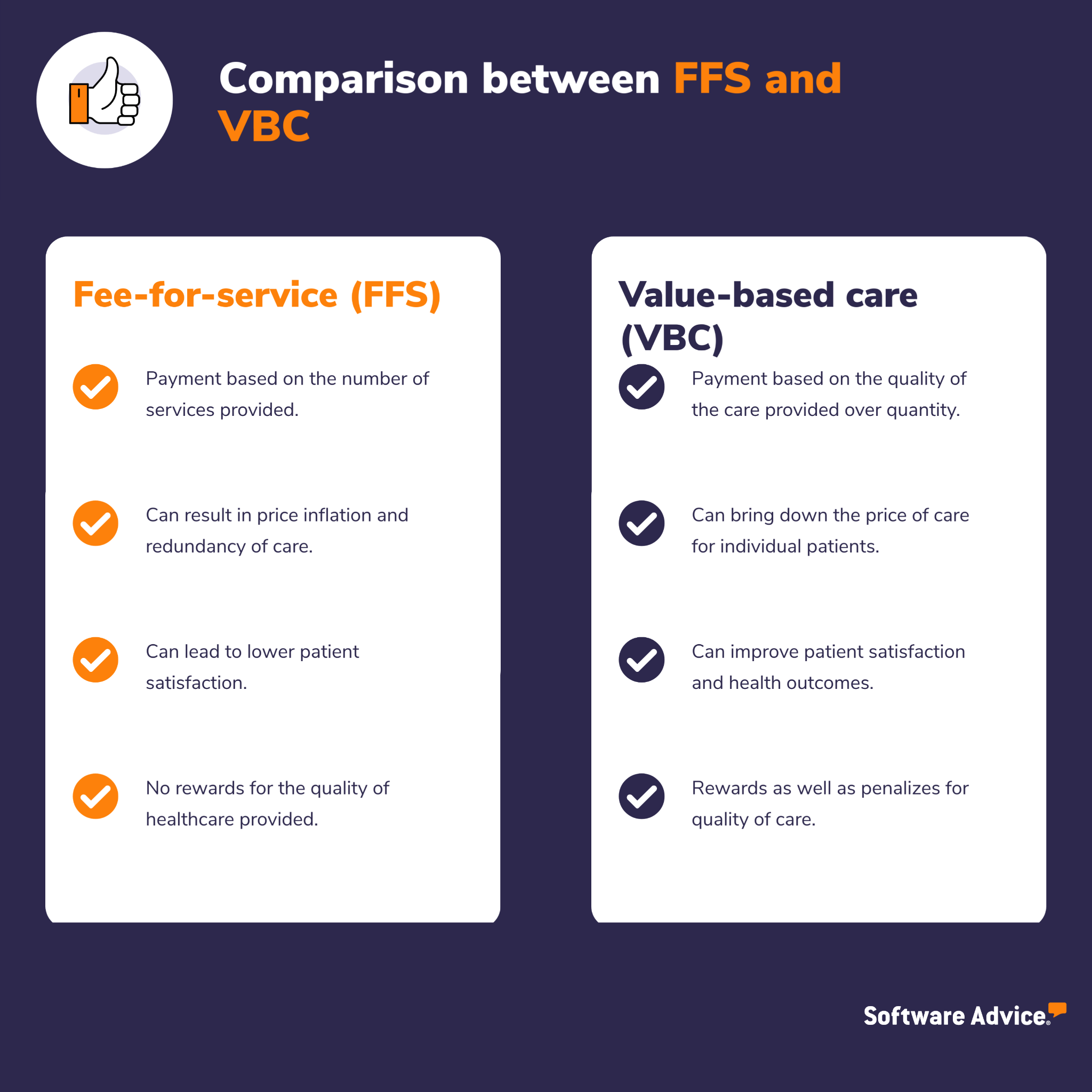
How is value-based care different from fee-for-service?
To reduce individual healthcare costs and improve patient outcomes, the government designed value-based care programs, which reimburse providers using numerous measures of care quality, instead of paying them per service provided.
That means value-based care is driven by data; providers have to track and report specific quality metrics to demonstrate improvement in patient health outcomes. Things such as hospital readmissions, adverse events, population health, and patient engagement during treatment are some of the metrics evaluated.
The value-based payment model rewards practitioners to use evidence-based medicine, engage patients more closely, upgrade health IT and medical software, and use data analytics to show proof of patient health improvement in order to get paid for their services.
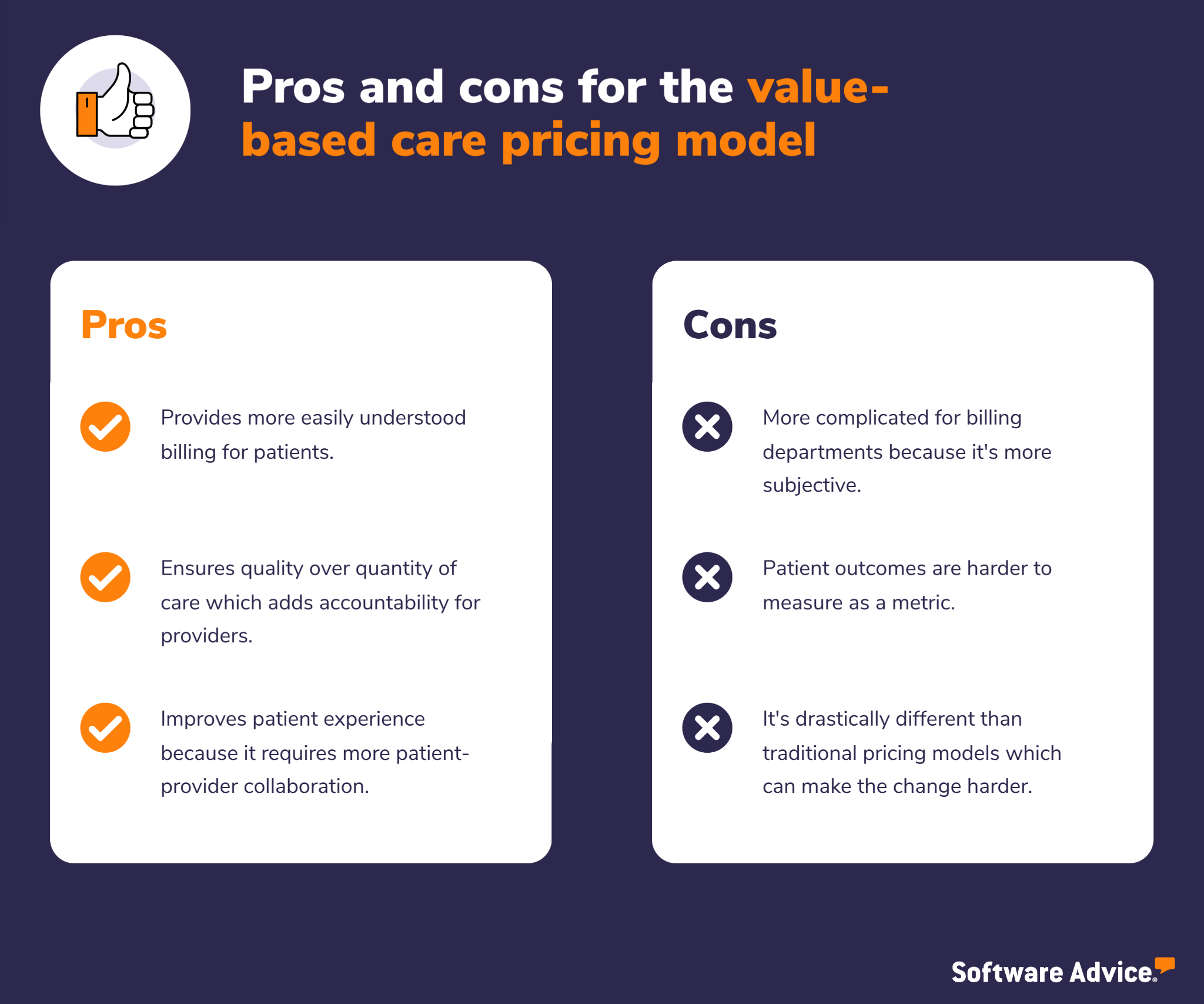
Pros of the value-based care healthcare model
Patients spend less money for better health care because value-based care doesn’t incentivize practitioners for throwing things at the wall to see if they stick. That means providers won’t benefit from recommending services their patients may not need or treatments that may not work, and that’s going to save patients money.
Additionally, providers are equipped to offer a better patient experience because a value-based model requires them to be more efficient and strategic with the care they offer during each patient visit. It rewards you for delving deeper into the underlying problems your patients may be experiencing instead of just running several tests, which can be costly, stressful, and uncomfortable for patients.
The doctor-patient experience is less transactional and more personal. During initial consultations, doctors and nurses spend time with their patients to get a more holistic idea about the reason for their visit. This improves the care experience for patients, as their needs are personally attended to.
Patients receive true value with their health care spending because traditional fee-for-service models incentivize doctor visits and prescriptions at their current prices, leading to inflated health care costs. Because of the high costs, many patients choose not to address their health issues until it’s too late or things have grown out of control, which becomes more costly in the long run.
By tying the cost of service directly to positive patient health outcomes, value-based healthcare helps lower the overall treatment cost for patients. It incentivizes doctors to be more thoughtful about what they prescribe and how they approach each patient. It also ensures physicians recommend only the most needed services, saving patients money on unnecessary tests or procedures.
Cons of the value-based care healthcare model
Although value-based healthcare is typically more beneficial for patients, it can be a hassle for practices because of the increased regulations placed on a healthcare provider. Because the government sets the terms of value-based care, it restricts how much you and your practice can do.
Additionally, because fee-for-service is so entrenched in the healthcare industry, it can be a tough sell for an entire healthcare organization to make the shift because of the uncertainty that comes with it. While it’s true that more providers are thinking of making the shift to value-based healthcare, the vast majority of practices and healthcare providers are still operating under a fee-for-service model.
That means that technology and infrastructure are still largely focused on accommodating that pricing model. You might also struggle to get buy-in from your staff and stakeholders because of the initial cost of making the shift from fee-for-service to value based healthcare.
Because billing is tied directly to quality of patient care, a provider needs to invest heavily in resources and software tools that are necessary to track important health metrics like hospital readmissions, adverse events, population health, and patient engagement during treatment. These are not typically monitored in a fee-for-service environment, so the tools your practice currently uses might not be sufficient to track them.
Why should your practice care about making the switch?
Fee-for-service is unquestionably the most widely used reimbursement method at the moment, but that won’t always be the case. In fact, more and more healthcare regulations are being rolled out each year to incentivize the switch to value-based care[1] because it’s cheaper for patients and insurance organizations. Additionally, insurance companies don’t have to pay as much for patient readmissions which means they are making more money, and patients are healthier and more equipped to manage their conditions.
The Affordable Care Act requires an annual, minimum 80% Medical Loss Ratio (MLR)[2] for individual and small group insurance plans, and an annual, minimum 85% MLR for large group plans. Congress imposed the MLR to provide greater transparency and accountability around the expenditures made by health insurers and to help bring down the cost of health care.
In addition to the ACA requirement, the Centers for Medicaid and Medicare Services (CMS)[3] is looking to push healthcare in the country toward total adoption of value-based care by 2030 which means more insurers are jumping on board early and adopting value-based care reimbursement.
If you don’t think value-based care or fee-for-service is right for your practice, you might want to consider concierge medicine or direct primary care. Check out our resources on those here:
Concierge Medicine Versus Direct Primary Care: Here’s Everything You Need To Know
A Concierge Medicine Guide: Definition, Salary, and Set-Up Info
Value-based care is the future of healthcare in this country, so you should adopt sooner rather than later
Aside from generally wanting to provide the best care for your patients as possible, the shift toward value-based healthcare is coming, so the sooner you and your practice hop on board, the better suited you are going to be to handle the organizational changes made by CMS and insurers.
Not only that, but your patient engagement and patient experience will increase which means you are more marketable to new patients and are much more likely to keep your current patients, resulting in less money spent on patient acquisition.
One of the key challenges you’ll face when making the shift is effectively tracking the metrics required to determine “value” in a value-based model. You’ll need to track staffing data, time and attendance of patients, clinical data, patient acuity data, and a bevy of other things to determine how to calculate cost of healthcare.
That’s where medical software comes into play. An electronic medical record (EMR) system, also known as an electronic health record system, can help your practice track and monitor patient health data from beginning to end. Additionally, you might want practice analytics software to help track key performance indicators to help justify the cost of making the switch.
Through one-on-one conversations and personalized recommendations, Software Advice guides you through your software search. In as little as 15 minutes, our software advisors can help you pick the right software for your business needs, so you can feel confident in your choice. Click here to chat with an advisor or schedule a call.
Sources
CMS Medicare Access and CHIP Reauthorization Act (MACRA), Centers for Medicare and Medicaid Services
Medical Loss Ratio Requirements Under the Patient Protection and Affordable Care Act (ACA): Issues for Congress, Congressional Research Service
Innovation Strategy Refresh, Centers for Medicare and Medicaid Services