What You Need to Know about Remote Therapy Monitoring
On January 1, 2022, the Centers for Medicare and Medicaid Services (CMS) approved reimbursements for remote therapeutic monitoring (RTM).
These new reimbursements are an exciting opportunity for healthcare providers and organizations to help expand remote care for their patients.
Practitioners who take advantage of these reimbursements by implementing a remote therapeutic monitoring program will see an increase in patient engagement, increase their healthcare organization’s revenue by over $200 a month per patient, and expand their ability to provide remote care.
Healthcare organizations that fail to implement a remote therapy monitoring program risk losing patients who are expecting greater attention to their needs. In the long run, this can cost the practice money and hurt their reputation.
If you’ve been thinking about implementing remote therapy monitoring but not sure where to start, we’re here to break down exactly what RTM is, how it’s different from remote patient monitoring (RPM), and the benefits you can reap.
Here’s what we’ll cover:
What is remote therapeutic monitoring?
Remote therapeutic monitoring allows patients to self-report data about their therapy response, medication adherence, musculoskeletal system status, and respiratory system conditions. They can either self-report how they feel or use a medical device (which can include certain medical software) that collects non-physiological data.
In general, remote therapeutic monitoring helps get more insight into patient conditions around these different issues:
Medication adherence
Virtual or distance physical therapy
Diabetes care management
Patient sentiment about treatments
Pain care management
Respiratory system care
For instance, a patient can record and narrate their medication adherence. They can monitor how they are reacting to the medication, how it makes them feel, or if it’s working the way it was expected to work.
Why remote therapeutic monitoring matters
Before CMS launched these new remote therapeutic monitoring CPT codes, practitioners weren’t as incentivized to interact with their patients about adherence to home exercise programs, but now that monitoring adherence is billable, practitioners can, and should, monitor and encourage home exercise programs that will help with chronic conditions.
Using just remote patient monitoring, practitioners would only see the data collected by the medical device out of context of the larger picture. Clinicians weren’t incentivized to dig deeper and ask about what might be driving those numbers.
With remote therapeutic monitoring, practitioners, like a physical therapist, get paid to ask patients to self-report data like exercise patterns, and how they’re feeling about their prescribed medication and exercise programs which adds much needed context to the data the remote physiologic monitoring medical device can provide.
Differences between remote therapeutic monitoring and remote patient monitoring
The primary difference between remote therapeutic monitoring and remote patient monitoring is that remote therapeutic monitoring focuses on monitoring health conditions like musculoskeletal system status, respiratory system status, medication adherence, and therapy response which allows for non-physiological data to be collected and reported.
Remote patient monitoring, on the other hand, requires all reported and gathered data (that is then digitally uploaded remotely) to be physiological like blood pressure, glucose levels, and respiratory system function.
With remote therapeutic monitoring, patients don’t necessarily have to use a medical device to report. They can share their perception of how they feel in relation to their treatment plans relative to past treatment plans. They can state pain levels after taking medication to better help doctors adjust medication levels.
These types of self-reporting weren’t incentivized using just the remote patient monitoring reimbursement codes, so it allows for more complete patient care.
If your practice already has a remote patient monitoring program in place, you should absolutely implement RTM services as well. The two programs go hand in hand and are intended to be used in tandem.
Benefits of remote therapeutic monitoring
Remote therapeutic monitoring comes with a variety of benefits for practices that choose to implement it.
Chief among them is the significant financial gains that practices and healthcare organizations can achieve. If your practice gets full reimbursement each month.-,What's%20the%20reimbursement%20amount%3F,non%2Dfacility%20national%20average).), you can earn $221.84 per patient per month with very little extra lift. In fact, a lot of the time, you would likely be doing billable actions already. It’s just a matter of understanding the new CPT codes and using them.
In addition to the financial gains your practice will see, remote therapeutic monitoring provides several valuable benefits to your patients:
Benefits
Higher patient engagement: Patients have more control over their health outcomes. Instead of blindly adhering to the medication or exercise regimen, they are in more constant contact with their provider to ensure they are doing things correctly.
Earlier intervention: Doctors have greater insight into their patients’ day-to-day activities and therapy adherence which leads to being able to identify warning signs if things aren’t working.
Reduced costs for patients: When patients and doctors work closely together to monitor chronic care management, patients are more likely to see positive outcomes which means less visits to the hospital.
Greater reach to underrepresented populations: Many Americans don’t live near complete healthcare facilities and might not have access to the care they need, but remote care helps better serve these underrepresented populations.
Patients have come to expect remote monitoring
A recent Software Advice survey* asked patients if they are interested in remote patient monitoring, and a vast majority said yes. Seventy-eight percent of patients with chronic conditions said they are “very interested” in sharing their health data remotely with their physicians.
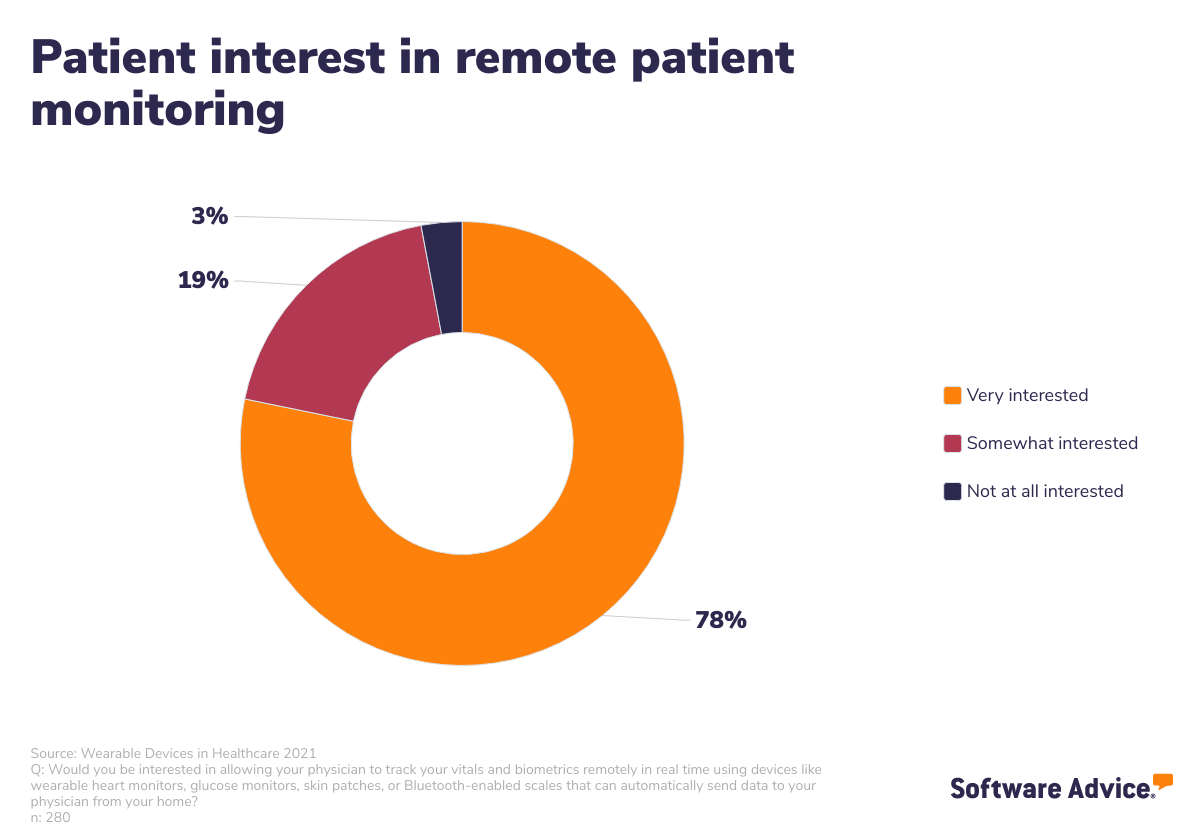
More than ever before, patients with chronic conditions are looking for, and expecting, their healthcare organization to offer some sort of remote monitoring. If your clinic has been hesitant to adopt remote therapeutic monitoring, this data might change your mind.
If you’re focused on improving the patient experience and increasing patient engagement, implementing RTM services or remote patient monitoring programs is a great start. To determine whether or not a remote monitoring program is right for your practice, start by running a patient survey to see if it’s something they would like. Also check the number of patients you have with chronic conditions.
Remote care is the future of comprehensive healthcare
Remote care, whether that’s remote patient monitoring or remote therapy monitoring, is becoming a must-have for practices that want to stay on top of providing the best care possible to their patients.
It’s also a no brainer. Remote therapeutic monitoring will help your practice increase patient medication adherence, respiratory system care, and pain, diabetes, and chronic care management programs.
Additionally, it’s an easy way to increase your practice’s revenue while also boosting patient engagement, reducing overall costs for your patients, and it helps you reach underrepresented populations more easily.
If you don’t have any remote monitoring services in place, check out our resources that include nearly everything you need to know to get started:
3 Benefits of Remote Patient Monitoring in Healthcare You Need to Know
4 Remote Patient Monitoring Reimbursement Tips for Your Practice
What Are the Remote Patient Monitoring Devices in Healthcare You Should Care About?
Methodology
Software Advice conducted this survey in August 2021 among 485 respondents to learn more about patient preferences and expectations for personal wearable device data and how it should be used by their healthcare providers. Respondents were screened for their location (United States) and how they kept track of their personal health history. For more information, see our methodologies page.