Interoperability in Healthcare: A Guide for Small Practices Choosing Software
Did you know that there are government-led incentives to simplify the process of sharing health data with patients and your colleagues, as well as benefits for your patients and practice whenever health data is more available?
Gartner [1] believes that the ability to share data and work between healthcare IT systems, along with the ability to compose and orchestrate new workflows outside of legacy or incumbent IT systems, will fundamentally redefine the healthcare provider’s application portfolio.
Put more simply, if you are a healthcare organization that focuses on interoperability, you will be able to provide greater service to your patients while also remaining more agile when it comes to shifting landscapes or turbulent, unforeseen problems.
Informed by Gartner insights [1], we’ve put together a list of things you should consider when evaluating your current tech stack in order to determine if you should increase or replace your software with more interoperable options.
What is interoperability in healthcare?
The official definition of interoperability in healthcare, according to the 21st Century Cures Act [2], is health information technology that:
Enables the secure data exchange of electronic health information with, and use of electronic health information from, other health information technology without special effort on the part of the user.
Allows for complete access, data exchange, and use of all electronically accessible health information for authorized use under applicable state or federal law.
This is a fancy way of saying it’s a piece of software that allows users to securely send and receive health information to and from other software, most commonly an electronic health record (EHR).
The U.S. government has recognized the potential value of interoperable medicine for a while now and has been working to incentivize providers to adopt interoperable practices through legislation and programs such as the HITECH Act, Meaningful Use, and MACRA.
According to Gartner [1], the megasuite vendor business model (when one vendor provides you with several different software solutions such as telehealth, patient portals, and an EHR all in one) depends on taking ownership of more and more adjacent IT spaces year over year through acquisitions. If every organization switches to using the same software megasuites, healthcare differentiation and agility becomes more difficult to achieve.
However, the megasuites are potentially stunting the adoption and growth of interoperable software solutions. Healthcare interoperability creates new opportunities to better coordinate and collaborate on care.
Benefits of interoperability in healthcare
The benefits of healthcare interoperability are substantial for both physicians and patients:
Save time by no longer waiting for paper records or test results to be faxed or scanned.
Collaboration between specialists means easier and better patient care coordination with fewer mistakes and misunderstandings.
Better communication means more positive outcomes and a reduced risk of malpractice lawsuits.
But how do you know your software is interoperable? And if it is, how can you start taking advantage of these features to see the benefits today?
The first step is to understand what interoperable software does. Then you’ll want to speak to vendors about the specific features they offer to accomplish these things.
The four fundamental functions of interoperable software
Interoperability can be a vague term, and while it has a clear definition, it’s hard to pin down what it looks like in terms of specific software functionality. Instead of trying to do that, approach it by understanding the crucial aspects of an interoperable system.
In order to be interoperable, your software must allow you to do the following:
1. Access healthcare data created by and stored in other systems
This generally translates to security-based features such as user logins and role-based access controls to manage who has permission to view and acquire patient data. You’ll also want auditing functionality to help keep track of who saw what healthcare data and when in order to protect your practice from HIPAA violations.
2. Share patient data created and stored in your own software with another system
This goes hand-in-hand with the first function, as interoperability means systems must be able to communicate with one another in both directions. Look for data selection options that allow you to know which patient’s records to send to other systems. You’ll also want your system to subscribe to standardized data entry.
For example, when sharing health information with other practices, you need to make sure you’re both using the same vocabulary and units of measurement to ensure there are no miscommunications.
Direct messaging is another great feature that enables exchange of health information between providers. It’s a great tool for simplifying these exchanges, so make sure it’s on your healthcare interoperability feature list.
3. Participate in health information exchange (HIE) programs
HIEs [3] are programs that help facilitate the secure data exchange of patient information in one of three ways:
Direct data exchange: Providers are able to send and receive secure patient health information directly and electronically to improve patient care coordination.
Query-based data exchange: Providers request secure patient information from one another.
Consumer-mediated data exchange: Patients are able to collect and control the use of their health information.
Interoperable software will, naturally, allow you to participate in these programs as they will be equipped to send and receive information to and from any other healthcare system.
If your software is interoperable, it should also be able to receive queries at any time of day and offer a record locator option to make finding and sending the requested information a simple and automated task.
4. Switch to a different system without losing any healthcare data
This is a big one. In order for a piece of software to be truly interoperable, the patient information collected and stored on it must be vendor-agnostic. By that, we mean access to the information cannot depend on what software you use.
To ensure this is the case, go back to the standardization of information. You need to make sure every piece of data collected on one system will look and read the same on another healthcare system.
What should you do about your current tech stack if it’s not interoperable?
While using all-in-one healthcare software megasuites can be more convenient, it can also hinder your practice’s ability to adjust and adapt to the changing healthcare landscape. Generally speaking, healthcare interoperability becomes easier to achieve if vendors are open with their application programming interfaces (APIs).
APIs allow two software components to communicate with each other using a set of definitions and protocols. A good example of this is how your weather app on your phone interfaces with the weather bureau’s software system which contains weather data.
Megasuites don’t typically like sharing their APIs, thus hindering the ability for these applications to communicate with each other in meaningful ways.
If your tech stack isn’t as interoperable as you’d like, you should consider looking for interoperable application ecosystems (IAEs). IAEs expose APIs for sharing information and functionality to form macro level workflows that can be orchestrated based on real-time data interoperability.
Put more simply, you want to look for smaller software systems and vendors who have mutual interests and are open to sharing their APIs. In general, IAEs offer a more practical, near-term approach to healthcare interoperability because, with an IAE, the whole is greater than the sum of its individual parts.
Putting it into practice
One example of what an IAE might look like is with care team collaboration. A care team will need four discrete software solutions to function:
Clinical communication and collaboration
Interactive patient care
Nurse call
Contact centers
What this might look like in practice is a clinical communication and collaboration vendor might interface or integrate with nurse call platforms to deliver on their value proposition. It becomes symbiotic and helps patients, vendors, and healthcare organizations to achieve their needs with greater efficiency.
This can also apply to other parts of your organization.
Putting it into practice
For instance, if you want to make sure your patient relationship management functionality is interoperable, you should find software solutions that openly communicate together to share this information:
Patient access
Customer resource management
Contact centers
Scheduling
Provider directory
The important thing to consider when seeking to improve your healthcare organization’s interoperability is to search for vendors who are willing to share their APIs to form IAEs. This means you need to look for vendors willing to cooperate with one another to share data regularly.
How to talk to your vendor about interoperability
After dipping your toes in the proverbial healthcare interoperability pool, you may find the benefits to be worth more of an investment, and that means talking to your vendors to find out more about the interoperability features they offer in their software.
You need to determine how/if your current software tech stack communicates and integrates with each other. Talk to your vendors to see if they are sharing their APIs with other vendors in order to make an IAE. They might not knowingly be participating in creating an IAE, but as long as they’re willing to collaborate and communicate, your software will be more interoperable.
To that purpose, we’ve created this list of questions for small and midsize practices to ask their current or prospective software providers in order to learn the same information:

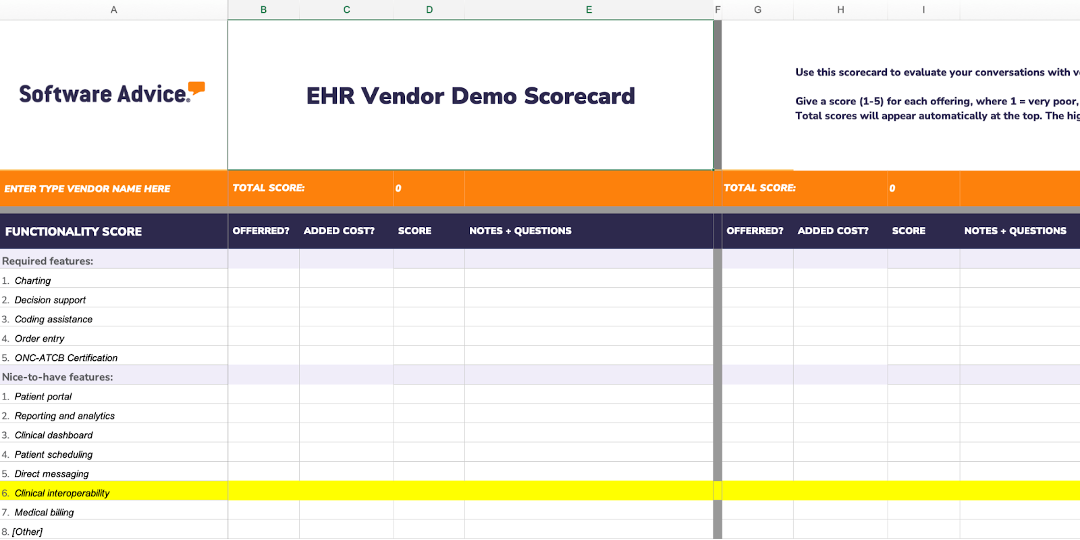
In addition to this list of questions, you can download the EHR vendor evaluation scorecard to help with your software selection process.
Interoperability in healthcare is still growing and evolving
While it is beneficial to your practice to jump on the interoperability bandwagon sooner rather than later, it’s still an evolving process that might not be immediately feasible for your practice. What’s most important is understanding what it is and that it will almost certainly become the norm in the future.
Looking for software?
We’ll help you find the right software for your needs and budget in 15 minutes or less for free. Schedule a call or click here to chat with a software advisor now. They’ll ask a few questions to learn about your needs, then provide a list of EHR systems that will work for you.
Sources
Establish Interoperable Application Ecosystems Early in Your Composable Healthcare Provider Roadmap, Gartner.com
21st Century Cures Act Documentation, Congress.gov
What is HIE?, HealthIT.gov