3 Predictions Defining the Future of Health Care Delivery in Small Practices
Small medical practices are always looking for ways to run more efficiently, so they can focus on delivering high-quality care and meeting patient expectations.
The best way to improve your efficiency is to learn about and adopt the latest advances in technology—but you may be unsure of what that looks like in practice. That’s why, in this article, we’re breaking down what you need to know about the latest technologies that are transforming patient care.
We’re focusing on artificial intelligence (AI), which has already made inroads into almost every industry, including health care. Many new technologies now leverage AI to enhance business operations, including the tech we’re covering here.
In health care, technologies such as chatbots and virtual assistants allow patients to instantly share their health data and receive more individualized attention. Data collected through these devices lets physicians and practices enhance their medical intelligence databases to offer the right patient care plans.
We predict that the technologies below will be the leading disruptors for small and midsize practices over the next three to five years. You need to start thinking now about how to incorporate them into your long-term health care delivery strategy to ensure you’re providing the best possible care to your patients.
Here’s what we’ll cover:
Predictive Analytics Assists in Accurate Patient Care
Conversational User Interfaces Improve Internal and External Processes
User Experience Personification Enhances Patient Retention
Predictive Analytics Assists in Accurate Patient Care
Predictive analytics digs deep into vast amounts of patient health data and suggests accurate outcomes for individual patients based on recommended care.
To do this, it uses statistical methods such as forecasting, regression analysis and pattern matching. The analyzed data includes past medical results, medical databases and the latest health care research from various journals.
What are the benefits for small practices?
Predictive analytics helps physicians identify at-risk patients. Early detection and intervention can help prevent various diseases, once patients are aware of urgent lifestyle changes they can make.
This technology also helps physicians make more accurate diagnoses and treatment plans.
For instance, when a patient comes in with chest pain, it’s tough for physicians to judge whether they should be checked in or sent home. In such a case, predictive analytics tools can help physicians analyze patient responses related to their exact condition and symptoms, by quickly referencing various medical literature sources, accessible databases and the latest scientific research, and then come up with an accurate assessment.
According to our “Top 10 Technology Disruptors for Small Businesses – 2018” report, by 2020, predictive analytics will change the way SMBs make decisions, causing a shift from mostly reactive decisions to proactive ones, across all industries and business functions.
In addition, Gartner predicts that: “By 2020, some form of predictive or prescriptive algorithm will be embedded in 75% of all health care delivery processes” (full content available to Gartner clients).
This means that the health care industry is set to become an algorithmic business in the near future, as predictive analytics and other advanced analytics models will make it possible for physicians to deliver faster and more accurate patient care, shifting the overall focus to prevention instead of treatment.
Here’s an example of what one practice experienced:
Predictive analytics helps reduce alert fatigue
New Jersey-based Virtua Memorial Hospital used predictive analytics to precisely identify patients who were at actual risk for postoperative respiratory depression and thus reduce the unnecessary number of irrelevant alarms that clinicians had to deal with.Pre-implementation: The top priorities of the hospital’s department of anesthesiology were to place better monitoring systems that detect respiratory depression early and create a safe environment for high-risk surgical patients. The department also noticed that patients suffering from obstructive sleep apnea are more prone to respiratory depression.
The anesthesiologists wanted to reduce the number of false alarms to help identify situations that actually need attention.
Post-implementation: The anesthesiologists used predictive analytics methods that considered variables such as pulse, oxygen saturation level and respiratory rate to detect signs of respiratory depression resulting from opioids among patients in post-anesthesia care.
The stakeholders examined multiple data sets through a multivariable rules engine to determine which alarms should be sent to the nurse-call phone system. As a result,
Alerts for respiratory depression were reduced by 99 percent, from 22,812 to 209.
The predictive analytics method alerted the clinicians as to which patients actually experienced real respiratory depression.
Recommended actions:
Start creating a strategy to build necessary skills: Consider partnering with local universities in your area and enroll your clinicians for analytics internships.
Prepare and test a predictive analytics infrastructure: Understand the power and potential of predictive analytics for accurate patient care. Implement a few change management procedures to ensure that the predictive algorithms you implement actually work. For instance, before applying predictive analytics directly in your intensive care unit (ICU) or other urgent/critical care cases, try using it as a way of preventing bottlenecks during peak patient visit times. You can use predictive analytics to monitor patient flow and schedule extra staff or make alternative arrangements for patients.
Conversational User Interfaces Improve Internal and External Processes
Conversational user interfaces include technologies such as virtual assistants and chatbots that allow users to experience digital interactions. These technologies are useful for both internal (e.g., managing repetitive administrative tasks) and external (e.g., customer service) purposes.
Artificial intelligence will be embedded in chatbots, virtual assistants and all other conversational user interfaces.
What are the benefits for small practices?
Conversational user interfaces have the ability to not only hold engaging conversations with a human but also assist them in various tasks.
When used internally, these interfaces make a physician’s job easier. For instance, a virtual assistant (VA) in a practice can assist physicians by answering routine patient queries, messaging patients and recommending treatment options. It can also manage many administrative tasks, thus reducing physician burnout.
When used externally, such as for patient engagement, these interfaces (e.g., chatbots) offer benefits such as instant online engagement with patients, because they’re available 24/7. They also increase the volume of online patient conversations, as many patients feel more comfortable discussing their health matters with a non-human.
By 2021, SMBs will implement conversational user interfaces in both internal and customer-related processes to enhance efficiency, according to our “Top 10 Technology Disruptors for Small Businesses – 2018” report.
In addition, a Gartner report (content available to Gartner clients) predicts that half of people under the age of 50 will rely on telemedicine and bots for routine care by 2022.
Here’s an example that shows you the benefits of a chatbot in a small medical practice:
Chatbots enhance patient response rate
Brett Swenson, M.D., based in Arizona, implemented a chatbot to improve patient engagement and successfully reached out to patients for his campaign on flu shots.Pre-implementation: During previous flu seasons, Swenson’s practice would send out emails and pamphlets to communicate with patients and remind them to get their flu shots. However, the patient response rate for these efforts usually stayed around 1 percent.
Post-implementation: Swenson decided to use chatbots to help facilitate better communication between patients and clinicians. He sent invitations to all his patients and saw the response rate go up to 30 percent. Patients also responded more quickly through the chatbot than through the other channels he’d used.
Recommended actions:
Start with a live chat tool: You can start your patient engagement efforts by adding a live chat tool on your practice’s website. You’ll need to designate one staff member to be available for this when it’s first launched. Later, you can transition the live chat offering into a full-fledged conversational user interface, i.e., a chatbot.
Implement knowledge management: If you’re unable to implement a virtual assistant for your physicians and staff now, you can prepare by setting up an internal knowledge management system. It centralizes your practice’s medical information, making it easy for physicians to find information quickly. In the future, when you do transition to a virtual assistant, you’ll find the knowledge management system useful for information access.
User Experience Personification Enhances Patient Retention
User experience personification is the process of implementing innovative ways to enhance the individual customer experience by adopting new technologies.
Medical practices must constantly develop and implement strategies that provide patients with a more personalized experience through technologies such as wayfinding solutions on mobile apps or bedside infotainment systems that include computer, television, phone and nurse call button.
Increased personalization experience usually affects patients’ behavior in a positive way, thus increasing the profit margins of medical practices due to revisits. You can create more personalized experiences by collecting and utilizing patient data.
What are the benefits for small practices?
User experience personification helps physicians identify the individual requirements of patients. Some of the benefits are:
Reduced stress and anxiety among patients due to technologies such as bedside infotainment systems that keep them entertained, thus increasing patient satisfaction and loyalty.
Reduced patient wait times as personalized appointments and reminders via text/email messages are sent for confirmed slots, thus enhancing practice efficiency.
Reduced staff interruptions as most of the experiential technologies eliminate staff involvement, thus allowing the staff to focus on other tasks.
Seamless patient experience via any device (mobile, desktop and kiosk).
By 2021, user experience personification will disrupt the personal experiences designed by SMBs in all industries, according to our “Top 10 Technology Disruptors for Small Businesses – 2018” report.
Gartner predicts that: “By 2019, 25% of health care providers will use experiential wayfinding to attract and retain patients and differentiate themselves in their markets” (full content available to Gartner clients).
Experiential wayfinding technologies sense and collect data, then analyze it to provide a unique patient experience. These technologies can be plugged into location-based services (such as Google Maps) and other advanced data analytics tools to collect data. For example, they can help patients navigate to the physician’s office and even assist them in finding their way around the facility once they arrive.
Another example of experiential wayfinding application is a parking management system that helps patients locate the nearest available parking spot when they visit a medical practice.
Experiential wayfinding helps patients navigate the halls of a medical practice facility
Kaleida Health, a western New York-based health care provider, implemented experiential wayfinding for a better patient experience so patients could navigate more easily within their facility.Pre-implementation: Kaleida Health’s patients and their families faced difficulty (lost the correct way and thus arrived late for appointments) while navigating within the practice’s newly opened facility, the Oishei Children’s Outpatient Center.
Post-implementation: Kaleida Health implemented experiential wayfinding in the form of a location mapping platform on its mobile app, MyKaleida. The app helped patients navigate within the new facility in a stress-free way.
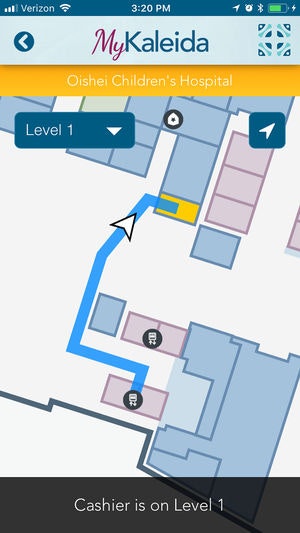
MyKaleida wayfinding via mobile app (Source)
The health care provider added high-fidelity maps to its MyKaleida mobile app that facilitated accurate turn-by-turn navigation to patients on its premises. It also helps hospital staff locate resources and deliver critical care.
Recommended actions:
Study existing use cases: To begin, you can study use cases to find medical practices like yours that are already employing user experience personification in some way. Ask your staff if they’re aware of any existing examples.
Start recording patient interactions: Start storing your interactions with patients in your EHR system, if you haven’t done so already. After that, you’ll be able to leverage persona information in the future through advanced data analytics tools.
Conclusion and Next Steps
The disruptors mentioned here will change the way medical practices operate in the coming years. Currently, large hospitals and health care providers have had a headstart in adoption and seen some success.
However, small practices should start preparing for these technologies now to enhance their long-term health care delivery process and remain competitive.
Here are few action steps to familiarize yourself with, or adopt these technologies:
Ask your EHR vendor about upcoming integrations, versions or solutions: Some EHR software vendors have already started to include AI-based technology integrations, such as predictive analytics, chatbots, virtual assistants and user experience personification into their products. Ask your vendor whether they provide any of the above technologies. And, if not, ask whether they plan to develop these features, or offer integrations with third-party solutions and any additional costs for those services. Based on their responses, you can set your business strategy to continue with the current vendor or look for a new one that offers these advances.
Talk to a software advisor: Before going for the most popular solution on the market, consult a software advisor and ask about products that specifically offer AI capabilities. Our medical software advisors will provide a free consultation at (844) 686-5616 so that you’re able to anticipate your needs better. They’ve helped thousands of small practices find the right solution. You’ll find it beneficial to identify which of these technologies you’ll need first and how you could incorporate it into your practice.