Everything Is Remote, Even Healthcare—Why Telemedicine Is Still the First Choice for 91% of Patients
At the onset of the pandemic, remote care delivery platforms were a unique and perfect solution for healthcare providers who needed to continue seeing patients while minimizing the risk of exposure to the virus. Even better was the fact that so many telehealth platforms already existed, were equipped with HIPAA-compliant features, readily available, and fast to deploy.
With a few quick changes to Medicare rules, telemedicine saw a huge climb in usage. But how do things stand now that we’ve settled back into a semblance of normalcy? Do patients still appreciate the benefits of telehealth, or have they grown tired of trying to connect with healthcare providers through a screen?
The answers to these questions should influence practices who have invested in telemedicine platforms, so we decided to find out.
91% of patients are more likely to select providers who offer telemed over those who don’t, making this tech critical for practices
We polled 1,002 patients who have used telemedicine to find out exactly how they feel about it, how the pandemic affected their use of remote healthcare, and whether or not they intend to keep using it.[*]
The short answer is that patients are still very happy with the benefits of remote care. In fact, our survey found that 91% of patients are more likely to select a provider who offers telemedicine over one who doesn’t.
What this means for providers: If you aren’t using telemedicine, or are considering getting rid of telemedicine now that the pandemic has settled down? You’re making a mistake.
Key findings:
86% of patients rate their experience with telemedicine as positive
70% of patients started using telemedicine during the pandemic, and over half (62%) say they prefer a telemedicine appointment when experiencing COVID symptoms
62% of patients still find the benefits of telemedicine valuable and prefer to consult with doctors remotely when possible
What kind of care do patients use telemedicine for?
Telemedicine, like any other medical tool, is a great way to treat certain patients and illnesses. It’s not perfect for every scenario, but it works incredibly well in certain situations such as video conferencing for therapy sessions and diagnosing common symptoms.
In order to identify the ideal telemedicine patient, we asked respondents to tell us how they’d prefer to receive care for a specific list of symptoms and illnesses.
Here’s what they said:
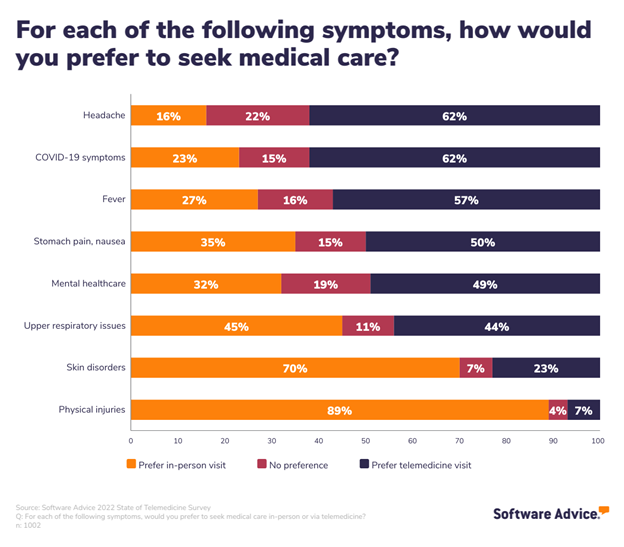
Common symptoms including headaches, COVID-19 symptoms, and fevers are much more popular options for virtual appointments.
It stands to reason that since these symptoms are so ubiquitous, patients feel they are easier to diagnose without requiring physical exams or labs. It’s also more likely that the illnesses associated with these symptoms are contagious, which makes remote care an even better option.
On the other hand, ailments requiring physical exams such as skin disorders (e.g., acne, rashes) and injuries (e.g., wounds, muscle strain, joint pain) are much more likely to send patients to a doctor’s office for treatment.
One area of particular interest here is the results around mental healthcare. This specialty is extremely well-suited for video conferencing, as generally no physical exam is required. Despite the fact that adoption rates among mental healthcare providers and patients have increased, patients in our survey were split fairly evenly among preference for this type of medical care.
The reasoning behind this is unclear, but it may be the fact that it’s easier for patients to feel a connection to providers they meet face-to-face, which in turn helps them feel more comfortable and able to open up.
The second factor we considered in our quest to identify the ideal telemedicine patient? Insurance coverage.
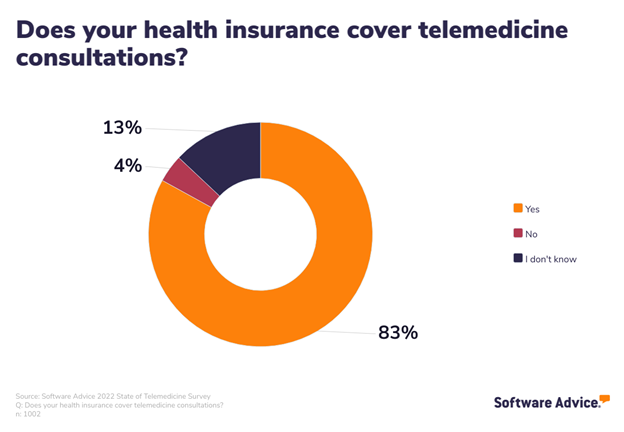
Fortunately, this includes most patients with some/any insurance coverage. At the beginning of the pandemic, the rules for Medicare patients were relaxed to include coverage for video consultations.
While the rules enacted by that legislation have all since expired, insurance coverage for telemedicine is still very common (42 states and DC require private insurers to reimburse for telemedicine).[1]
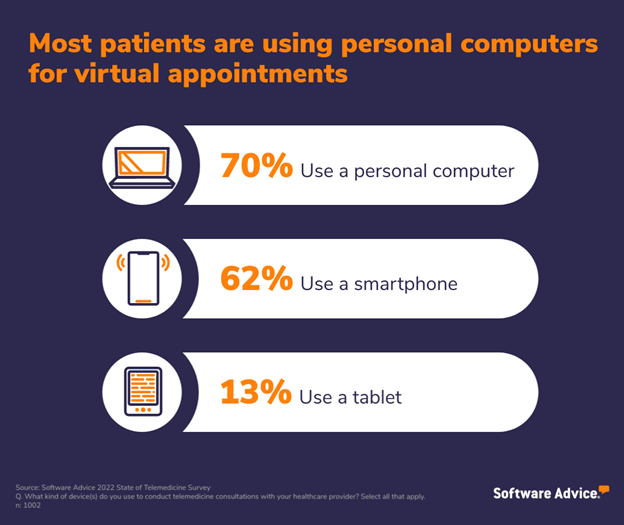
The final factor that makes a patient well-suited for telemedicine is access to video-capable technology and other remote patient monitoring tools.
Only three respondents in our survey said they use landlines for these remote consultations, which illustrates the value of video technology for remote consultations. Patients want to be able to see their doctor’s face while speaking to them, if possible.
Patients are primarily using personal computers (70%), smartphones (62%), and tablets (13%) for their virtual appointments.
Taken together, these findings paint a picture of the ideal telemedicine user; the candidate who is best-suited for remote care, and the providers who are most equipped to provide that care via video conferencing tools.
The ideal telemedicine user is someone with:
Mild and common symptoms,
Insurance coverage, and
Access to video-capable tech
Telemedicine had pros and cons, but 86% of patients are happy with it
In terms of general likes and dislikes around telemedicine use, surveyed patients have overwhelmingly positive things to say.
We know that patients are happy with their telemedicine experiences, as 86% rated them positively in our survey, so it’s good to start out recognizing that any complaints patients have about remote care are relatively minor.
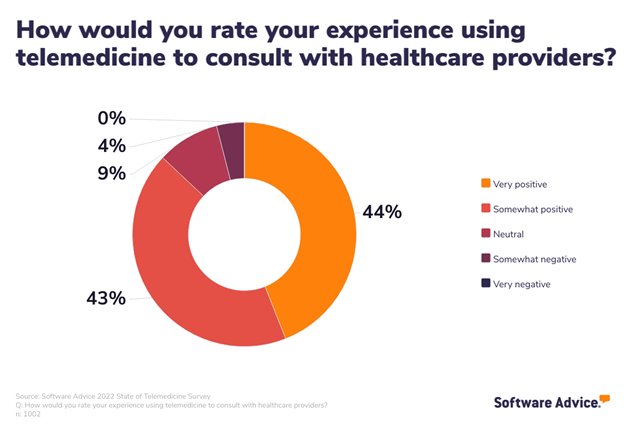
While just under 10% of respondent experiences were neither positive nor negative, the big takeaway here is how incredibly skewed the responses are toward positive experiences—only four percent say theirs was “somewhat negative,” and a grand total of zero patients chose “very negative” for this question.
Additionally, we asked patients about any concerns they had regarding quality of care received via telemedicine appointments.
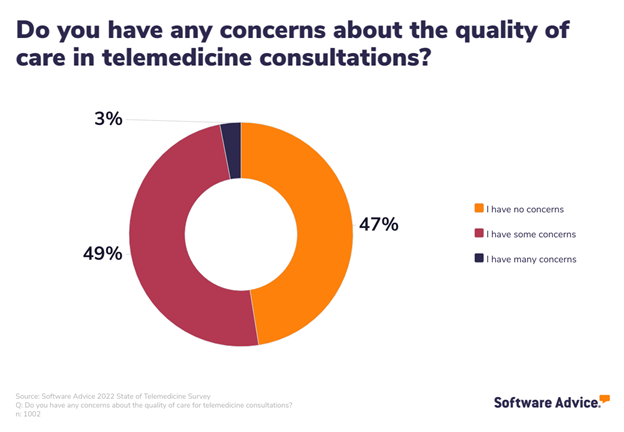
While about half of patients expressed some concerns, a nearly equal number said they have none whatsoever.
When taken together, these two statistics lead us to believe that the issue is tied to messaging. By communicating more clearly exactly how telemedicine appointments go and what steps providers are taking to ensure patients get the same quality of care remotely as they do in-person, patients’ concerns will lessen.
Considering the circumstances that led to the widespread, rapid adoption of telemedicine services within the past three years, we wanted to find out exactly what led patients to try it. The biggest motivating factors? Convenience and ease of use.
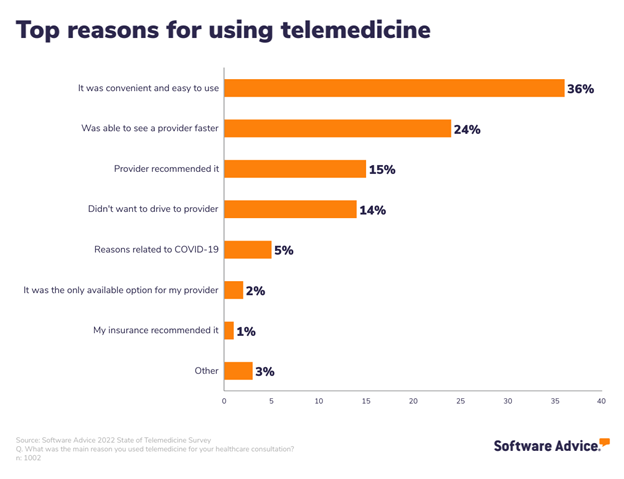
Another quarter of patients used telemedicine because they were able to connect with their healthcare provider faster with a virtual visit than if they scheduled an in-person appointment.
We also asked about the general pros and cons of telemedicine. While every respondent in our survey has something positive to say about telemedicine, 33% experienced no negatives to speak of.
The biggest benefits for telemedicine use among patients were similar: The ability to receive care without having to drive (39%) and in the comfort of their own home (35%).
This shouldn’t surprise anyone, considering the rise of remote work, curbside order pickup, and delivery services in the past three years. People, not just patients, are growing more and more accustomed to convenience, so much so that it’s becoming an expectation. And what’s more, the definition of convenience has evolved to include not having to leave the house.
Telemedicine provides a golden opportunity for healthcare professionals to tap into that.
Apart from the third of patients who have had no negative experiences with telemedicine, another 33% called out the inability to receive an in-person or physical exam via remote consultation.
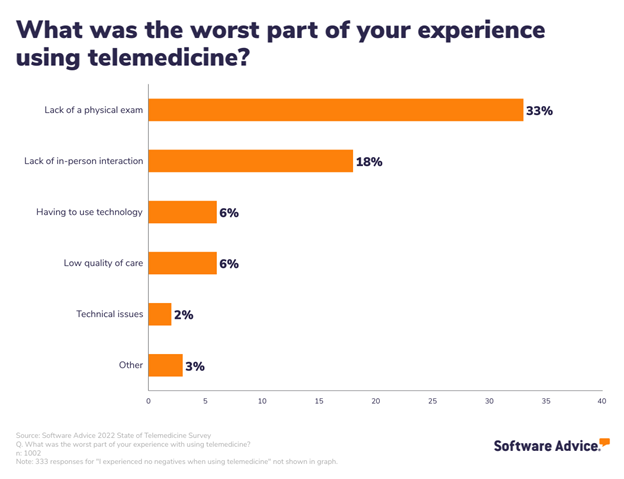
This is obviously the biggest drawback for telemedicine as a whole, since some medical conditions require a physical exam, lab work, or other testing that must be done in-person to diagnose. We saw this issue bear out in other areas as well (we’ll get into that in the next section).
There are, of course, some solutions for this lack of physical proximity. Patients can acquire their own biometric recording tools, such as blood pressure cuffs and thermometers, to collect that data and share with providers during video consultation. While that’s not ideal for everyone, it does help identify the ideal telemedicine user.
Wearable devices are a modern marvel. But have you considered the patient perspective when prescribing medical wearables? Read our research.
How the pandemic affected telemedicine use, and where we go from here
To figure that out, we started by assessing how much the pandemic had to do with patients trying telemedicine for the first time; this turned out to be the case for 70% of patients.
Another 14% say that while they had used telemedicine before March 2020, their use of these remote consultation tools significantly increased during COVID. (We did ask if any patients saw a decrease in telemedicine service use during the pandemic, and only one respondent selected that option.)
But patients are only half of the equation when it comes to telemedicine users. After all, providers have to use these tools to see and treat patients remotely as well.
In an effort to understand their perspective and better inform our understanding of patients’ experiences with telehealth, we ran a separate survey of over 150 healthcare providers.[**]
In this second survey, providers echoed some of the same sentiments from our patient survey. For example, most providers adopted telemedicine during the pandemic, but continue to use it to see patients remotely to this day.
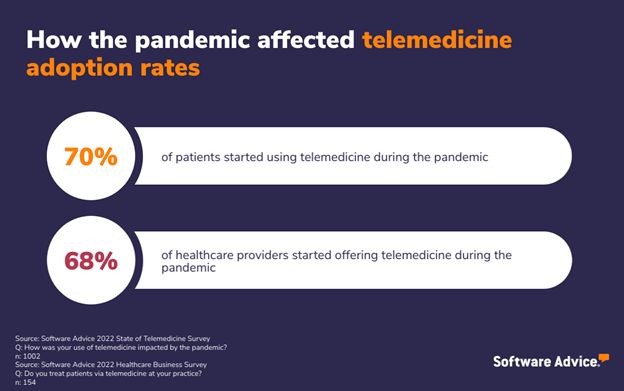
So the evidence is clear here: Telemedicine adoption rates were significantly impacted by the pandemic.
But will they stay up as we move out of it? All signs point to yes.
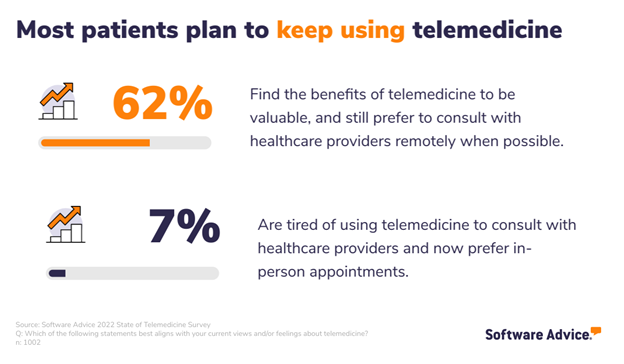
Over half of patients said they find the benefits of telemedicine to be valuable, and they continue to prefer video consultations with their doctors when possible.
Another third of patients don’t feel strongly either way, and only seven percent are tired of using telemedicine and prefer in-person appointments from now on.
Here again, provider feelings mimic patients’. We asked doctors in our second survey how they feel about using telemedicine, and over half (62%) rate their experience as positive. Only 16% say their experience was negative.
We also wanted to know how telemedicine availability affects patients looking for new doctors. Are they more likely to choose a provider who offers telemedicine over one who doesn’t?
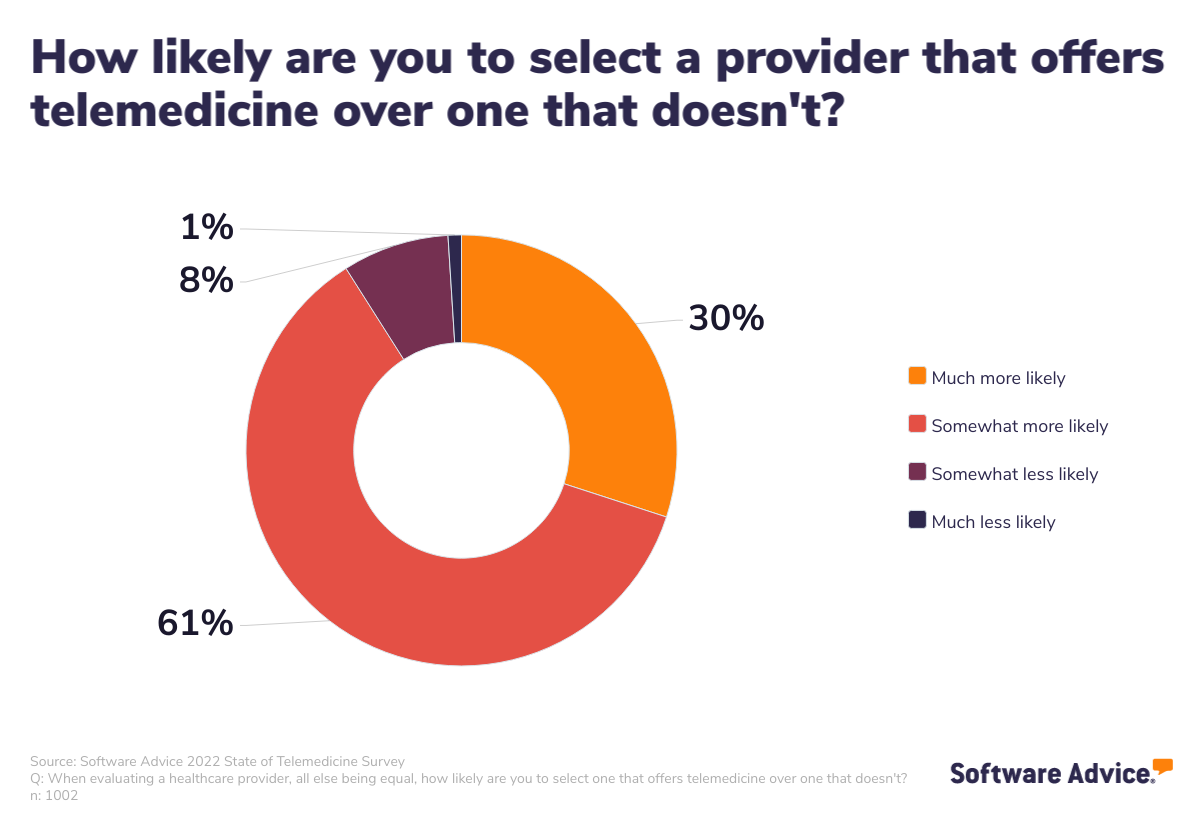
Again, it’s a resounding yes.
An astounding 91% of patients say they’re more likely to go with a doctor who has a telemedicine option over one who doesn’t.
Bottom line: Telemedicine is here to stay
So, what does all this mean for providers? The answer is clear: Patients have grown to appreciate the convenience, flexibility, and simplicity of telemedicine. If you are a provider who implemented a remote system in the early days of the pandemic, keep doing what you’re doing.
Patients are still happy with it, so now isn’t the time to abandon that practice.
In fact, you should double down on that investment. Consider running patient surveys to see how your patients feel about the telemedicine platform you’re using—are there any easy improvements you could make to increase convenience? Should you upgrade to a more robust platform? Your users are best-suited to answer those questions for you.
If you’re a provider who has managed to avoid telemedicine up to this point, your hesitation is unfounded. Our advice is to find a system that works for you, and start the process of video consultations as soon as possible.
You’ll likely want to start out with a system that offers the most basic functionality, including:
Secure video conferencing
Instant messaging or chat
Virtual waiting room
Appointment/schedule management
A great place to start is our FrontRunners, which compiles data from product information and user reviews to create a shortlist of the top products on the market.
Survey methodology
* Software Advice conducted the 2022 State of Telemedicine Survey in August, 2022 of 1002 respondents to learn more about telemedicine use and how it has been affected by the pandemic. Screening questions were used to narrow respondents to those with relevant experience with the subject matter.
** Software Advice conducted the 2022 Healthcare Business Survey in August, 2022 of 154 healthcare providers to learn about business trends and struggles that are affecting the operation of their practices right now. We used screeners to ensure we were speaking to providers who would have relevant knowledge and experience with the topics addressed, including limiting job titles to doctors, nurses, and office administrators.
Sources
1. Private Insurance Coverage for Telehealth, TELEHEALTH.HHS.GOV