Physician Burnout in the Pandemic Age
You probably already know this, but the situation healthcare workers are currently facing is dire.
Physician burnout caused by the conditions of working in a pandemic is forcing huge numbers of medical workers to leave their jobs, and hospitals are facing a shortage of nurses and workers as their beds remain full.
We’ve talked about physician burnout before, back in 2018 and again in 2019, because it was an issue even then. But it’s all too obvious that the current circumstances are creating a much more significant level of burnout among healthcare workers than we’ve ever seen before.
Like we said, dire.
But we can’t just shrug our shoulders and give up, or walk away from medicine entirely and hope for the best. Doctors have to keep treating patients, and we have to find a way to make that job easier for them to do.
To that end, Software Advice surveyed a group of healthcare professionals—207 family and general practitioners and 50 mental health therapists—to understand their experiences with burnout during the COVID-19 pandemic and to try and figure out what strategies actually work to mitigate the stress of treating patients during this time.
The pandemic’s impact on physicians
One of the most compelling stats we found was that over half of physicians and therapists in our survey have considered early retirement or a career change to escape pandemic-related burnout.
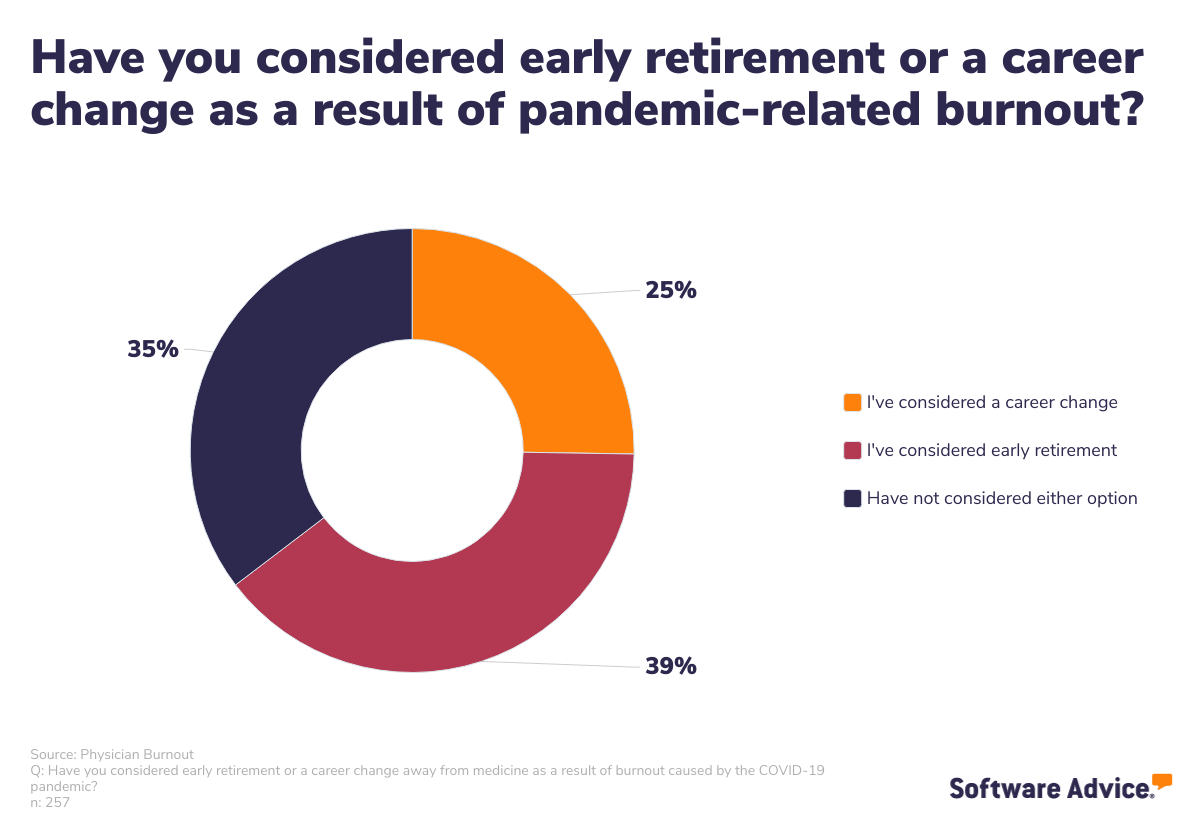
The mass exodus from healthcare is real, and it’s alarming. There was already a shortage of qualified healthcare professionals before the pandemic, but the added deficit is going to have serious consequences, including making healthcare harder to access, more expensive, and less effective.
This hammers the point even harder: Healthcare employers must find ways to bring relief to their workers as quickly as possible. But the first step is understanding exactly how the pandemic is affecting providers.
Burnout symptoms experienced by providers
We asked our survey participants to tell us how often they experienced certain symptoms traditionally related to physician burnout and found that emotional exhaustion and changes to sleep patterns were the most frequent.
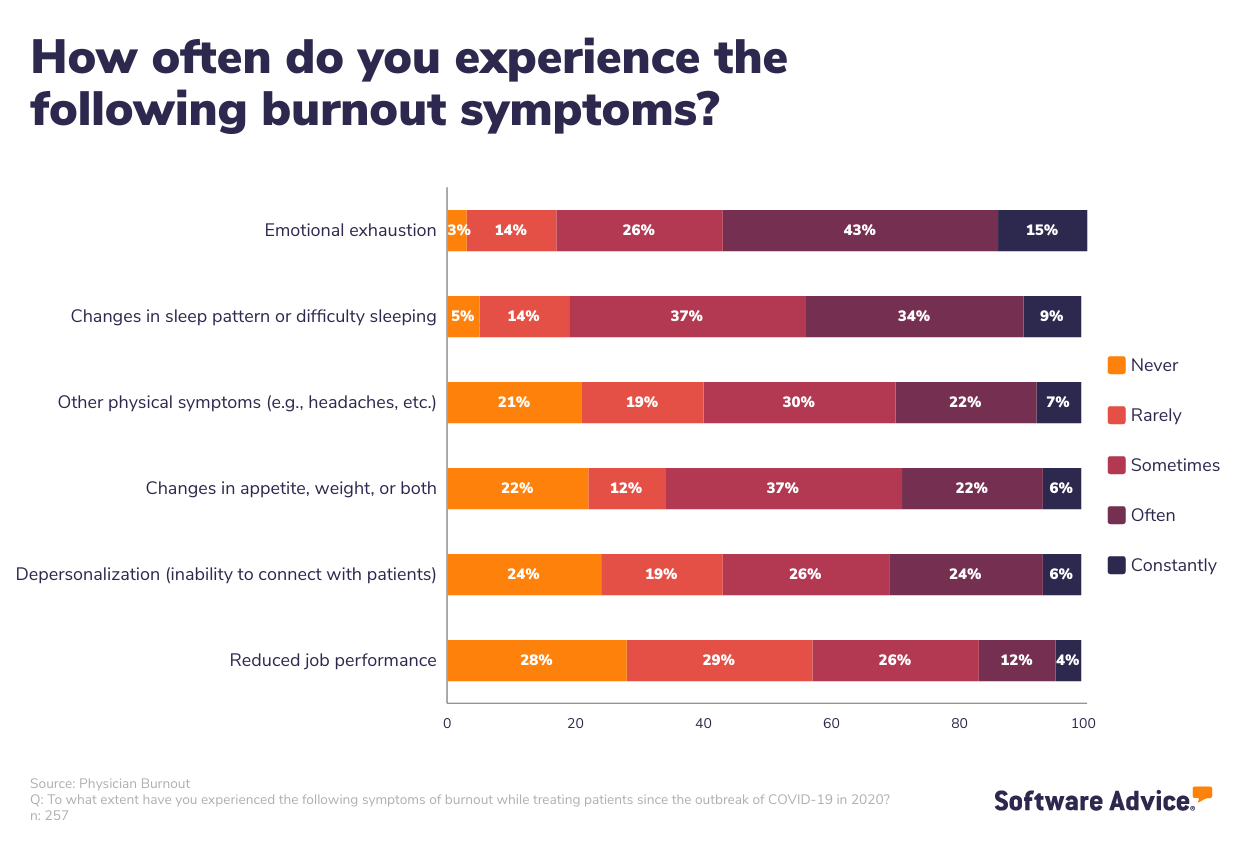
Three-quarters of respondents reported feeling depersonalization, or an inability to connect with patients, at some point, with 30% saying they experienced this symptom “often” or “constantly”.
Which brings us to our next critical issue with physician burnout: It has a detrimental effect on healthcare providers’ ability to provide adequate patient care.
The impact of physician burnout on patients
We asked physicians and therapists what specific aspects of treating patients led to an increase or acceleration in burnout. Here’s what they said:
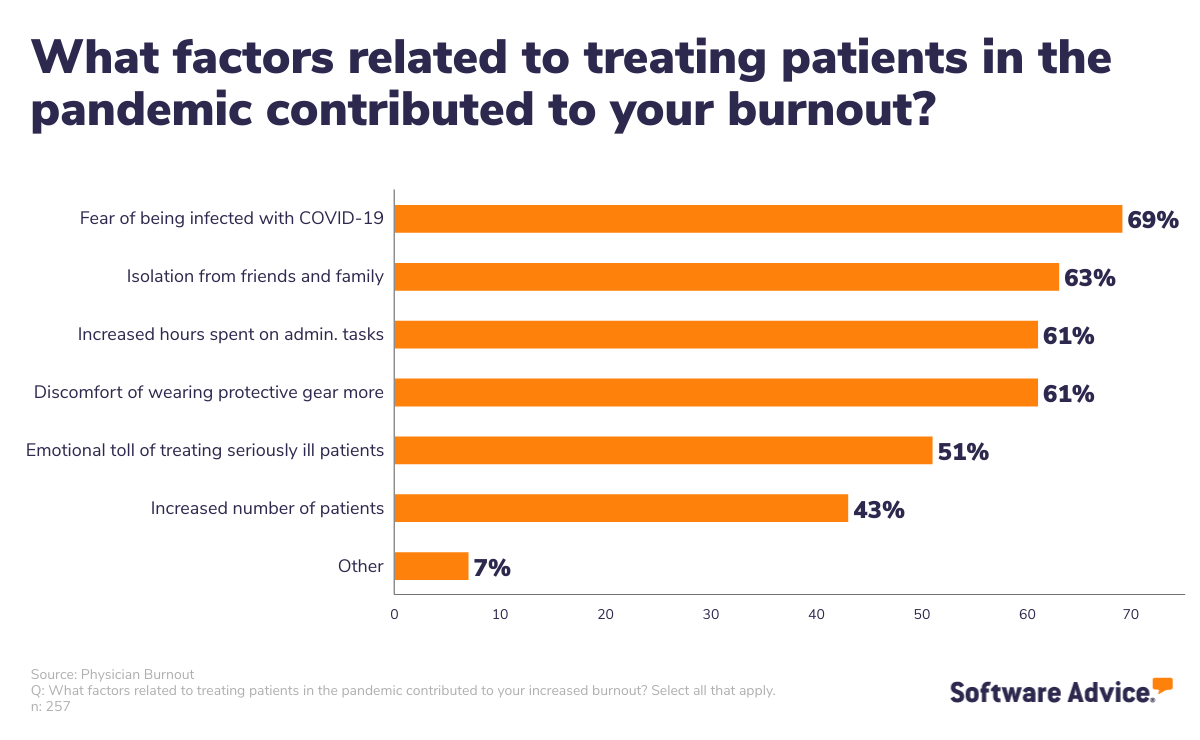
The leading factor was a fear of being infected with COVID-19 themselves, followed by isolation from friends and family. We also collected open-ended responses from those who chose the “other” option here, and an interesting—yet not entirely surprising—theme emerged.
Here are a few of those write-in responses:
“Time spent educating resistant patients about COVID and vaccination.”
“Patients’ complete ignorance.”
“Patients being accusatory and blaming doctors.”
“Fielding questions about COVID-19, resistance from patients regarding masks, vaccines, etc.”
“Politics and distrust in science/medicine. Disrespect to medical providers.”
“Patients’ attitude changes.”
There is a sense that the public has turned on healthcare providers, and the betrayal cannot be overlooked as a root cause of the extensive burnout we’re seeing now. The detrimental impact on healthcare providers’ mental health is difficult to overstate.
We also asked respondents how doctor burnout has affected their practice and ability to treat patients.
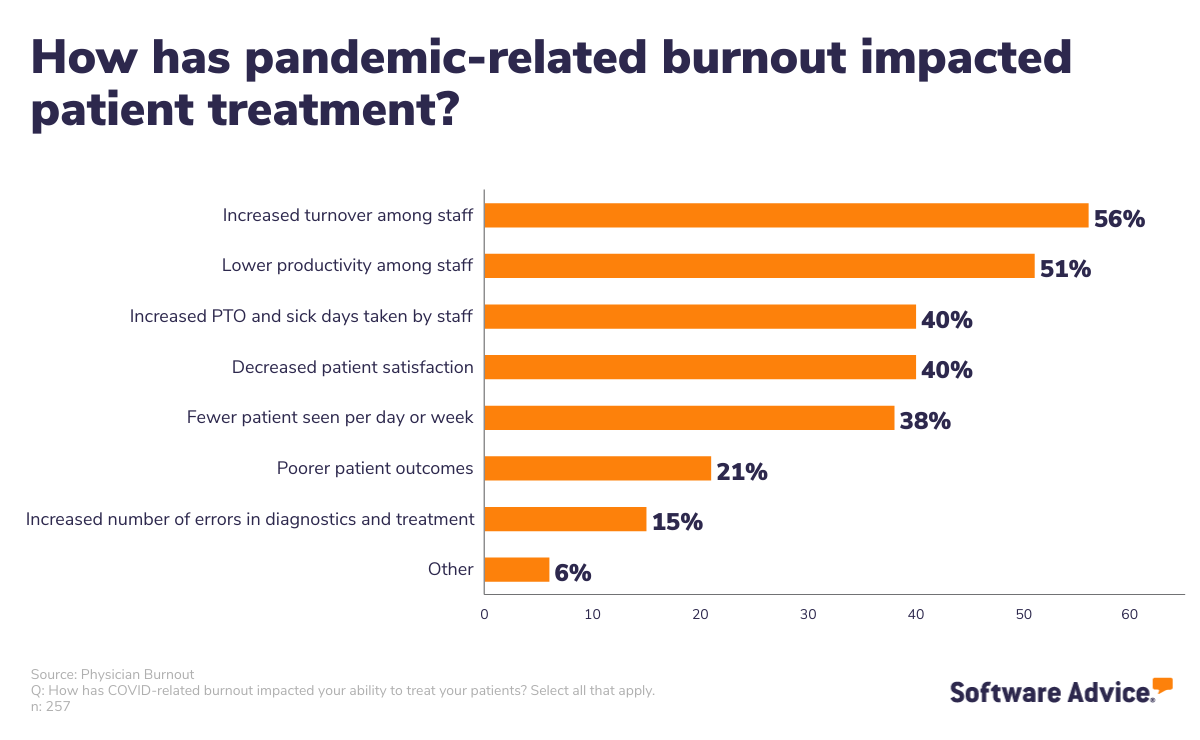
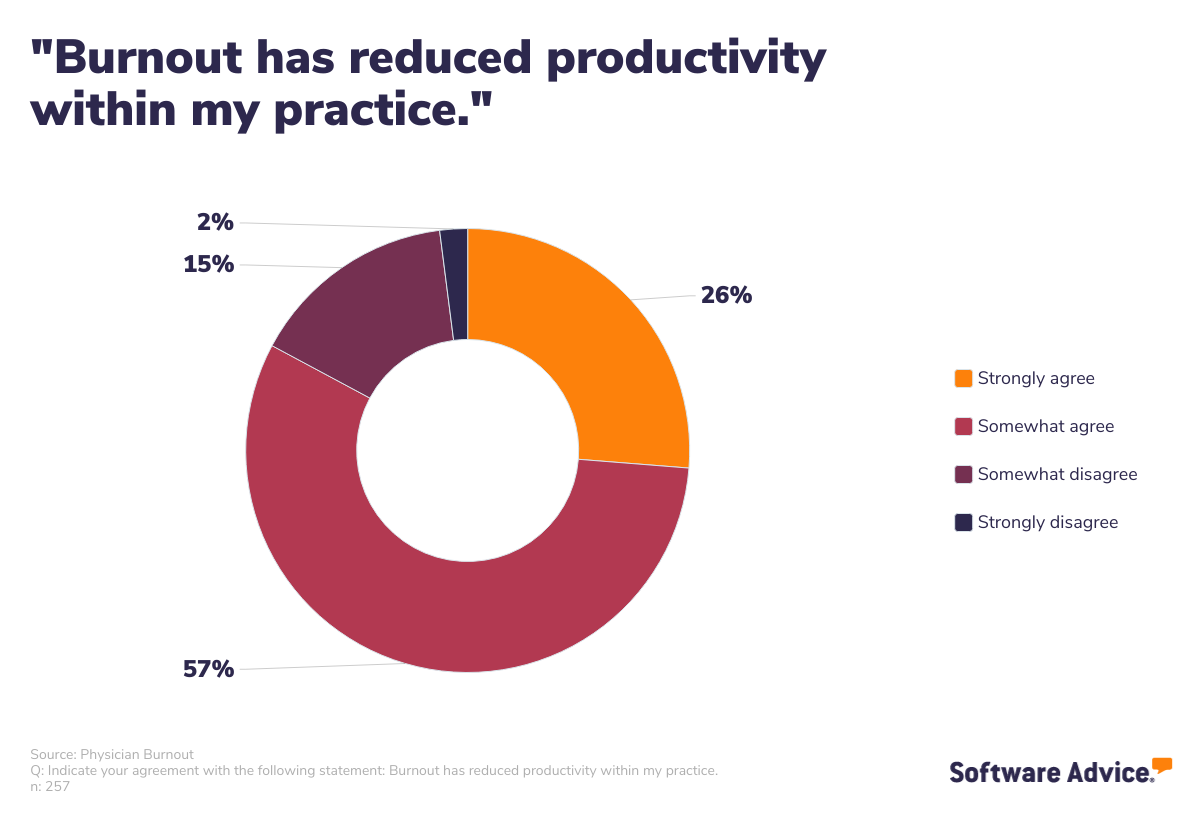
Unsurprisingly, there’s a high rate of turnover among healthcare staff at the moment. This further evidences the fact that healthcare workers are leaving the profession in droves. We also found four out of five respondents agreed with the sentiment that burnout has reduced productivity.
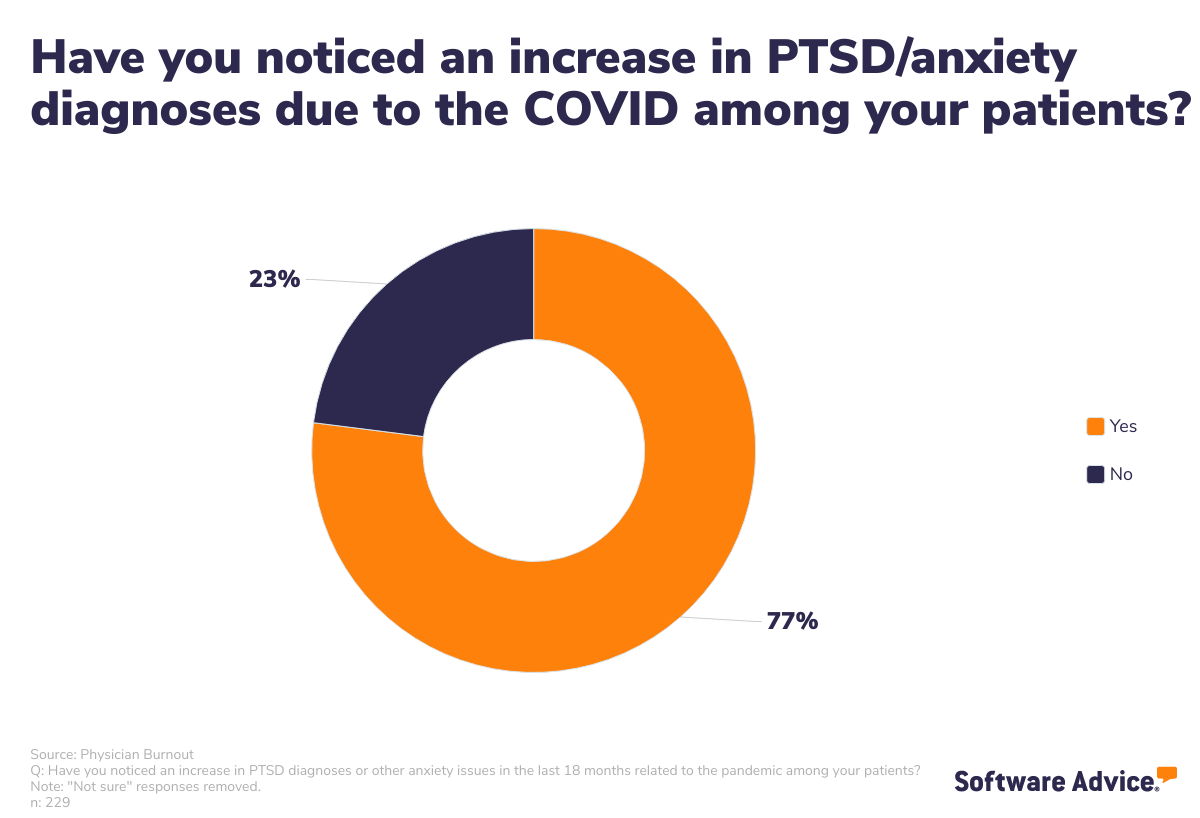
In addition to the indirect impact of covid on patient safety by reducing physicians’ ability to adequately treat them, the COVID-19 pandemic is also taking a serious toll on their mental health. We asked our survey respondents if they’ve noticed an increase in PTSD or other anxiety diagnoses related to the pandemic in the past 18 months among their own patients; over three-quarters said they had.
We spoke to Dr. Amanda Hilberg, a Staff Psychologist and Clinical Supervisor at Austin Anxiety and OCD Specialists with a background in areas of OCD, Generalized Anxiety Disorder, Panic Disorder, and Insomnia, among others, to find out if this matched what she’s seeing in her own practice, and it is.
“I have witnessed increased severity of both anxiety and post-traumatic stress symptoms.
Patients experiencing obsessive compulsive disorder have expressed heightened concerns about disease contamination. I have seen elevated social anxiety due to isolation and lack of opportunity for consistent social interaction. The lack of travel and concerns about disease transmission have deepened driving and flying phobias.
Unsurprisingly, the pandemic has also amplified agoraphobia and panic symptoms. Both anxiety and post-traumatic stress disorders are marked by avoidance of feared stimuli (certain places, people, activities, objects, etc.), and during the COVID-related isolation of the past 18 months, many of these avoidant behaviors have been reinforced and strengthened to the point where my patients are experiencing difficulty functioning in several domains of their lives.”
So, long story short: The prolonged pandemic is having an increasingly negative effect on everyone who participates in healthcare. That’s well established. What’s less obvious is how we can combat clinician burnout to try and improve the situation for physicians and patients.
To answer that question, we explored what measures medical practices have already taken, and how providers felt about them.
What’s being done about burnout
Right now, there’s a two-pronged approach to slowing the burnout rate among healthcare workers. Individuals are taking responsibility for their own mental health and wellbeing by adopting strategies in their personal lives to fight stress, and employers are providing some resources to help their staff better deal with the pandemic and its impact in their professional lives.
Strategies for individuals
Awareness around mental health and stress management has grown in recent years, but never has it been more important for individuals—especially those working in medicine—to practice healthy ways of coping with stress than right now.
We asked our survey participants what self-care techniques they’ve adopted since the pandemic began to help deal with burnout.
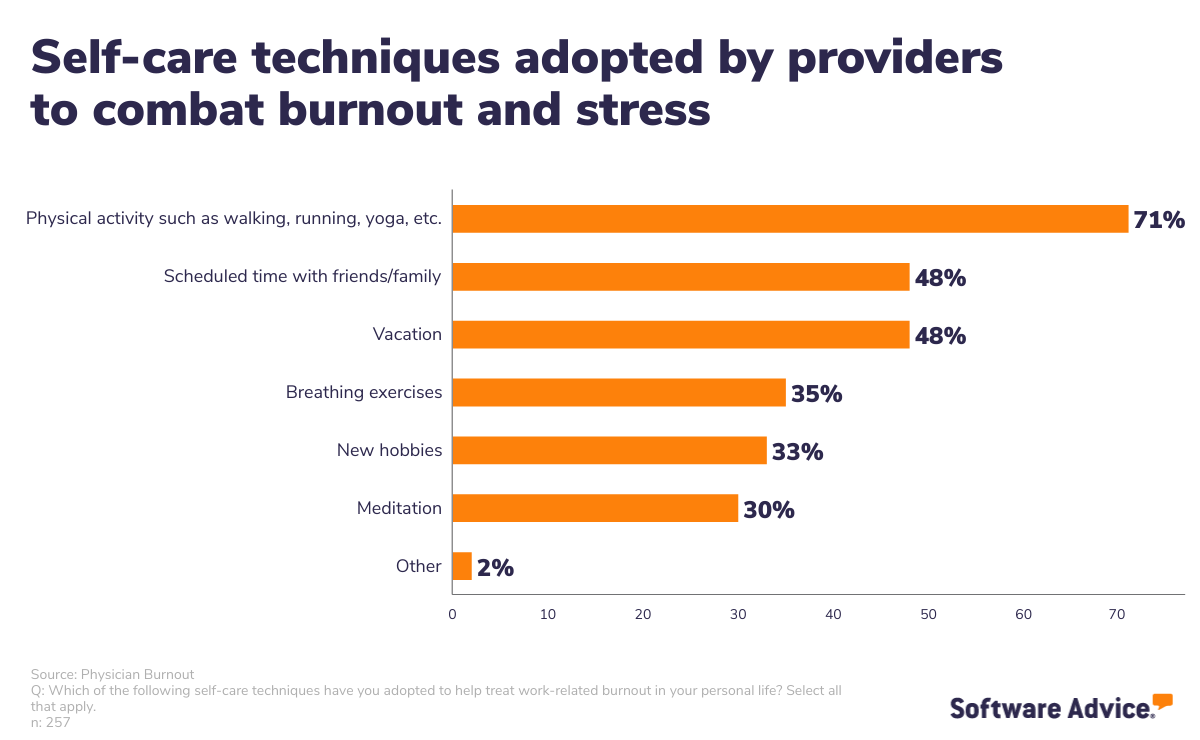
Physical activity was the top response, and for good reason. It’s well documented that moving the body can have a positive impact on stress levels, and it’s safe to say most healthcare professionals are well aware of that fact.
Dr. Hilberg had additional recommendations for self-care techniques healthcare professionals can adopt on their own time to better manage stress:
“Combining physical activity with other mental health coping techniques provides a more comprehensive approach to dealing with the difficult emotions healthcare workers experience on a daily basis…While there are many more techniques that could be helpful, the two specific skills that I’ll often introduce are mindfulness exercises and self-compassion practices:
Mindfulness activities help individuals momentarily pause and redirect their focus back to the present, away from their future or past thoughts or trauma reminders. Three evidence-based mindfulness activities that I use in my practice quite often are diaphragmatic breathing, progressive muscle relaxation, and grounding exercises.
Self-compassion, as defined by Kristen Neff, PhD, ‘entails being warm and understanding toward ourselves when we suffer, fail, or feel inadequate, rather than ignoring our pain or flagellating ourselves with self-criticism.’ This is easier said than done, but is a skill that can be cultivated with practice and perspective.”
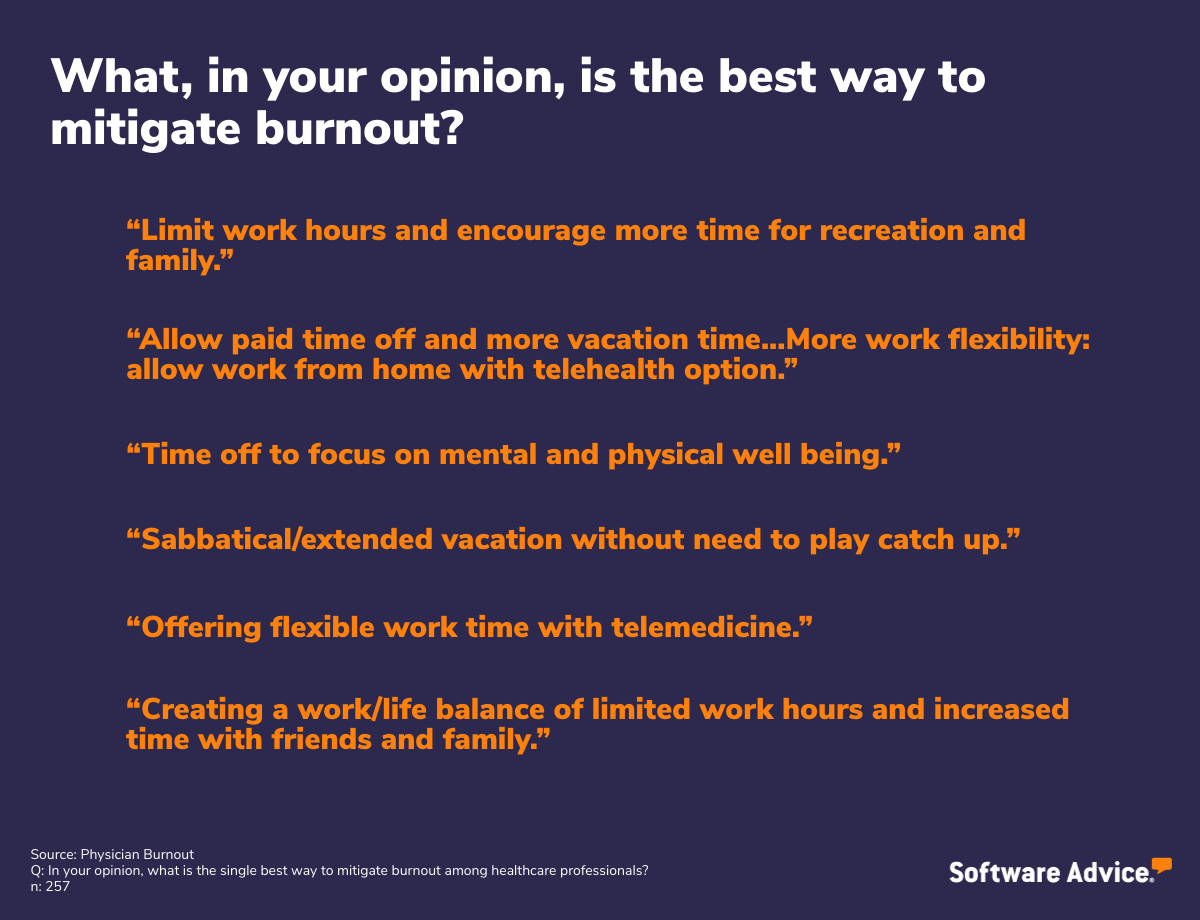
We also asked all our respondents what, in their opinion, was the single best thing that would help mitigate burnout among healthcare workers. With limitless possibilities for answer responses, 34% mentioned more paid time off or flexible work hours.
But this takes us away from things healthcare workers can do on their own and into the strategies their employers need to adopt to better support them through this pandemic.
Strategies for employees
We asked the doctors in our survey what measures have been taken by their practices to mitigate stress and burnout. Here’s what we found:
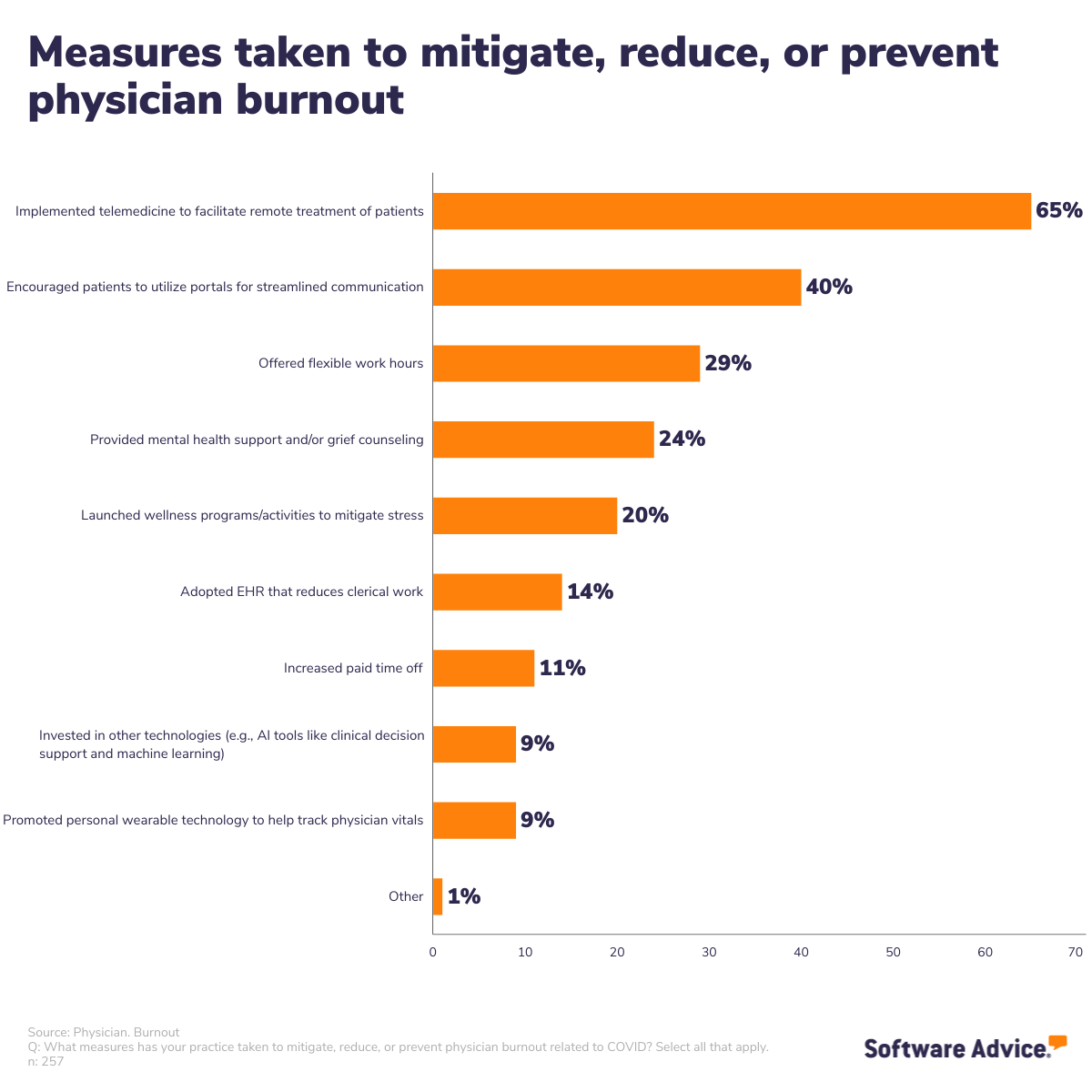
The top two responses were software-related, with number one being adopting a telemedicine system to facilitate remote delivery of care, followed by patient portals to enable better communication between providers and patients.
Interestingly, the following three measures were ones our respondents called for in their open-ended answers above: flexible work hours, mental health support, and wellness programs.
But did these measures actually have an impact on burnout? We asked respondents to tell us that as well:
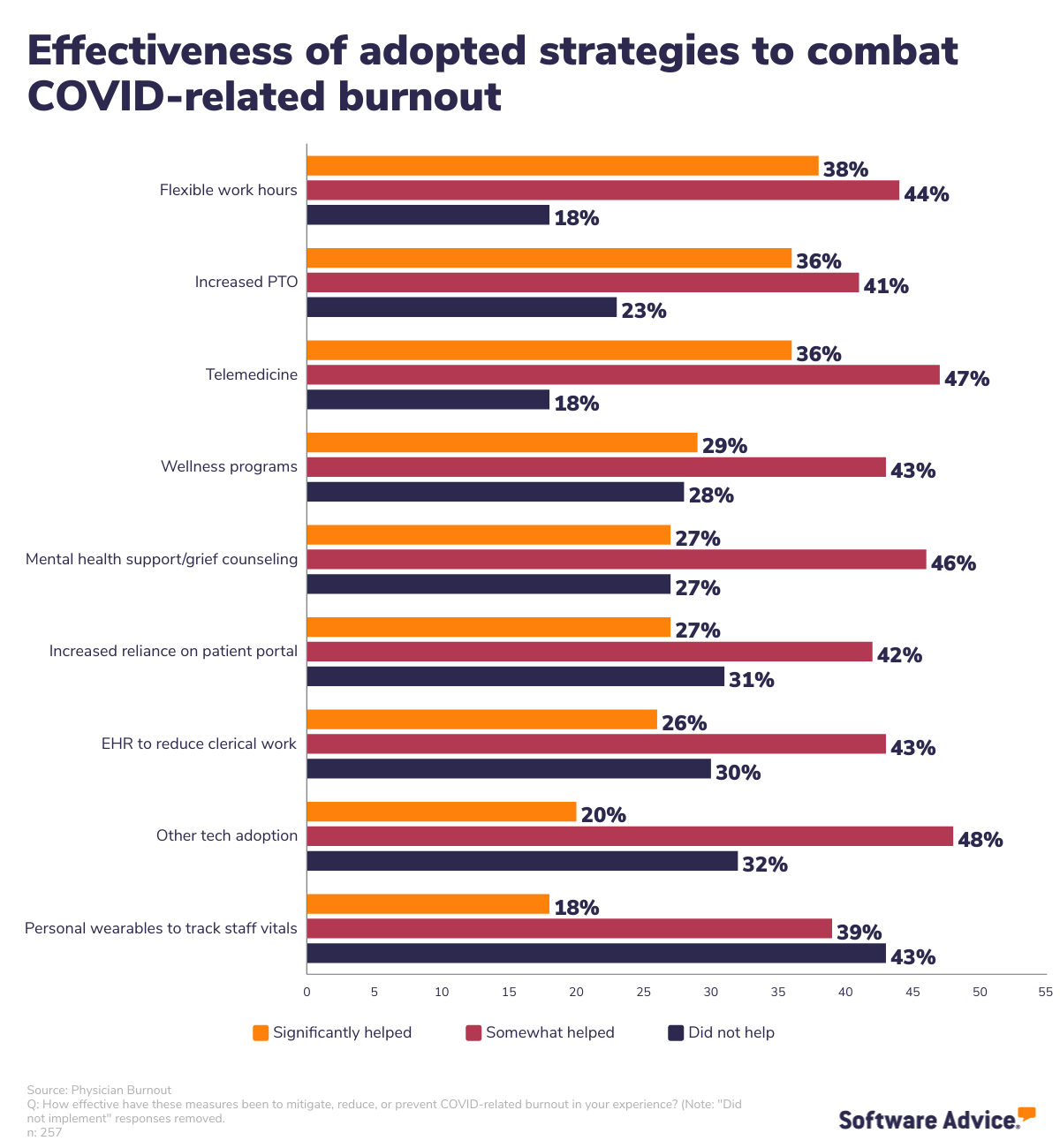
According to doctors working at practices that adopted these measures (those that did not adopt were removed from the data), flexible work hours and increased paid time off were the most helpful measures taken by employers to mitigate burnout.
Dr. Hilberg concurs:
“Both mental health support and flexible work hours could be helpful in that both can foster a sense of enhanced autonomy and control.
Key elements of burnout (per Dr. Patricia Grabareks) include feeling disconnected from other, non-work aspects of life, emotional and/or physical exhaustion, and feelings of inefficacy. These concerns are highly interconnected, and providing mental health care and flexible work hours for employees can help alleviate some of those burnout factors.”
What should be done about burnout
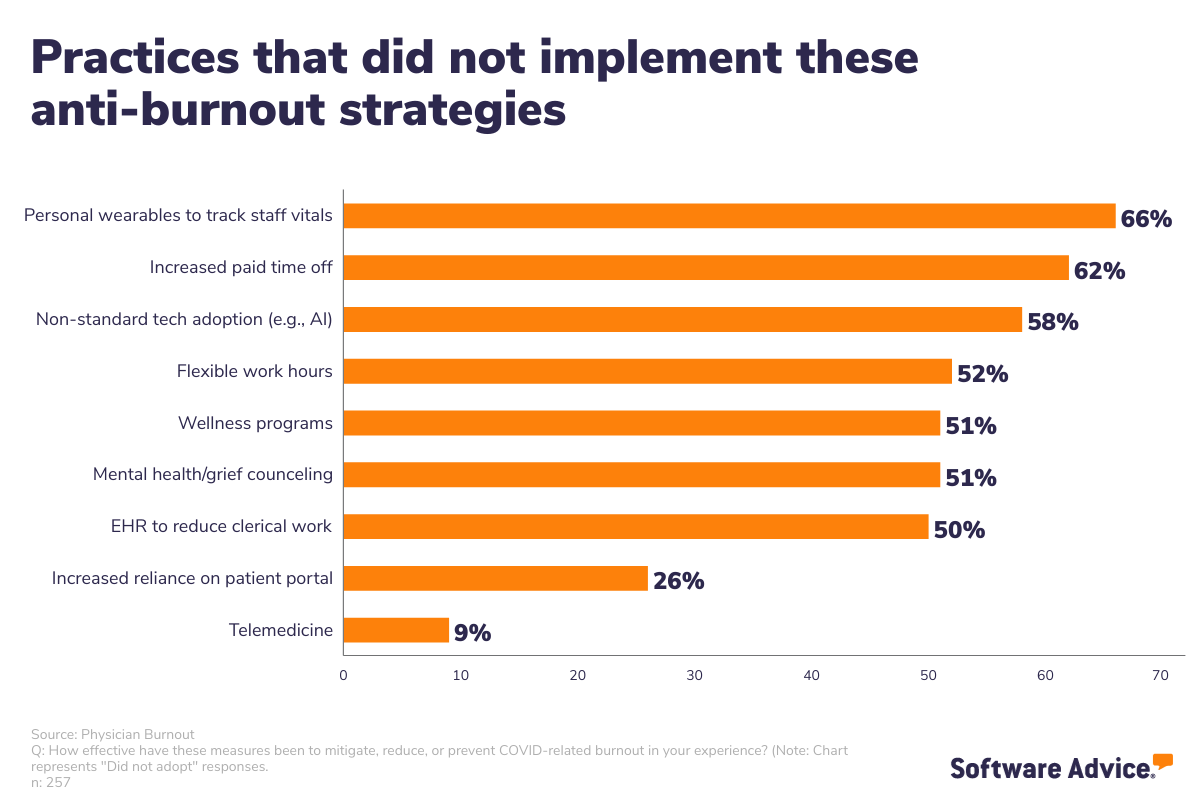
We’ve already talked about strategies to help mitigate stress and make the lives of doctors easier, and each is certainly worth consideration. We discovered that, even though doctors found certain measures helpful in combating their burnout, plenty of practices have not yet adopted them.
Per Dr. Hilberg, it’s up to employers to alleviate as much of the burdens causing burnout as they can:
“I believe that the most effective strategy to better manage these concerns is to have empathetic leadership that is open to eliciting feedback about employee needs and taking actionable steps based on those needs. Companies must practice what they preach about wellness in order for their employees to thrive.”
Solution 1:
Employers and practice owners can start with more obvious policy changes, like flexible work hours and more paid leave, to make their healthcare workers’ lives better right away.
It is not entirely a simple action to take, considering the shortage of healthcare workers; however, evidence shows that employers must bring relief to their employees right away otherwise they risk losing even more staff. A practical solution would be to reduce your practice’s hours of operation, making it easier to limit employees’ working hours and manage schedules of reduced staff. This is, hands down, the right choice to make.
Solution 2:
Invest in wellness and support programs. Do everything in your power to combat the stigma of healthcare professionals speaking to therapists. There’s a real fear among medical doctors that seeking therapy will jeopardize their professional licenses, and that’s simply untenable. It’s apparent that doctors and healthcare workers are hurting right now, and they need support from their administrations.
As one respondent in our survey put it, “Revamp the system…Treat that root cause and don’t blame doctors for ‘lack of resilience’ when we are being abused.”
Solution 3:
Push vaccine advocacy. This is, unfortunately, a very touchy recommendation because vaccinations have become political rather than factual. But the truth remains, no matter how many people call it opinion: Vaccines are the way to end the pandemic.
Evidence from our survey shows that doctors are frustrated by patients ignoring their advice and the scientific studies that prove COVID vaccines are safe and effective. It may be time for this issue to become an administrative one rather than the responsibility of each individual doctor. With hospital beds filling up and emergency care practices running ragged, administrations may have to consider turning away COVID patients who had an opportunity to get vaccinated but refused.
The bottom line:
Healthcare providers need support right now. That can manifest in several different ways (see solutions 1-3 above), but they are all asking for the same thing from their employers. Now is the time to exercise understanding and compassion to healthcare employees as much as possible, or practices risk exacerbating the worker shortage and hurting themselves and patients a lot more in the long run.
Physician Burnout Survey, 2021
Software Advice conducted this survey in August, 2021 of 257 healthcare providers to learn more about pandemic-related burnout and how healthcare providers should address burnout. Respondents were screened for general and family practitioners (207) and mental health therapists (50) currently working in U.S. practices with 20 or fewer licensed providers.
Note: Interview responses have been edited for brevity and clarity.