The Ultimate Guide to Value-Based Care for Medical Practices
Healthcare organizations and practices are always looking for ways to improve the patient experience while reducing the cost of service. That’s why the type of patient reimbursement model you choose for your practice is important.
Most providers use a fee-for-service (FFS) model, which incentivizes physicians based on the number of services provided instead of the quality of care. But value-based care, one of the newer reimbursement models, seeks to change the way patients receive healthcare, ultimately resulting in various benefits for everyone involved.
In this article, we explain what value-based care is, how it’s different from traditional reimbursement models, and how both your patients and your practice can benefit from adopting a value-based healthcare model.
Here’s what we’ll cover:
How is value-based care different from other models?
What are the key types of value-based care models?
Benefits of adopting a value-based care model
What is value-based care?
Value-based healthcare is a pricing model that incentivizes your practice based on the quality of services you provide to patients. Within a value-based care model, your practice is compensated depending on a patient’s health outcomes. The more traditional FFS model, on the other hand, pays based on the number of visits, tests performed, and prescriptions administered.
Value-based care puts more emphasis on ensuring healthcare providers like you take care of patients’ medical needs in as few visits as possible and to the best of the physician’s ability.
The goal of a value-based care system is four-fold:
Improve the quality of healthcare
Improve the patient experience
Lower costs for patients
Improve the care team’s experience
How is value-based care different from other models?
Under FFS models, medical practitioners are incentivized to see as many patients as they can as quickly as they can. They’re paid per service, which means the more tests and procedures they prescribe to patients, the higher they get paid.
Since the focus is on the number of services, patient care tends to get ignored. Physicians spend less one-on-one time with the patients and prescribe more tests without getting to the root of what patients may be experiencing, thus impacting the overall health outcome.
To reduce individual healthcare costs and improve patient outcomes, the government designed value-based care programs, which reimburse providers using numerous measures of care quality, instead of paying them per service provided.
That means value-based care is driven by data; providers have to track and report specific quality metrics to demonstrate improvement in patient health outcomes. Things such as hospital readmissions, adverse events, population health, and patient engagement during treatment are some of the metrics evaluated.
The value-based payment model rewards practitioners to use evidence-based medicine, engage patients more closely, upgrade health IT and software, and use data analytics to show proof of patient health improvement to get paid for their services.
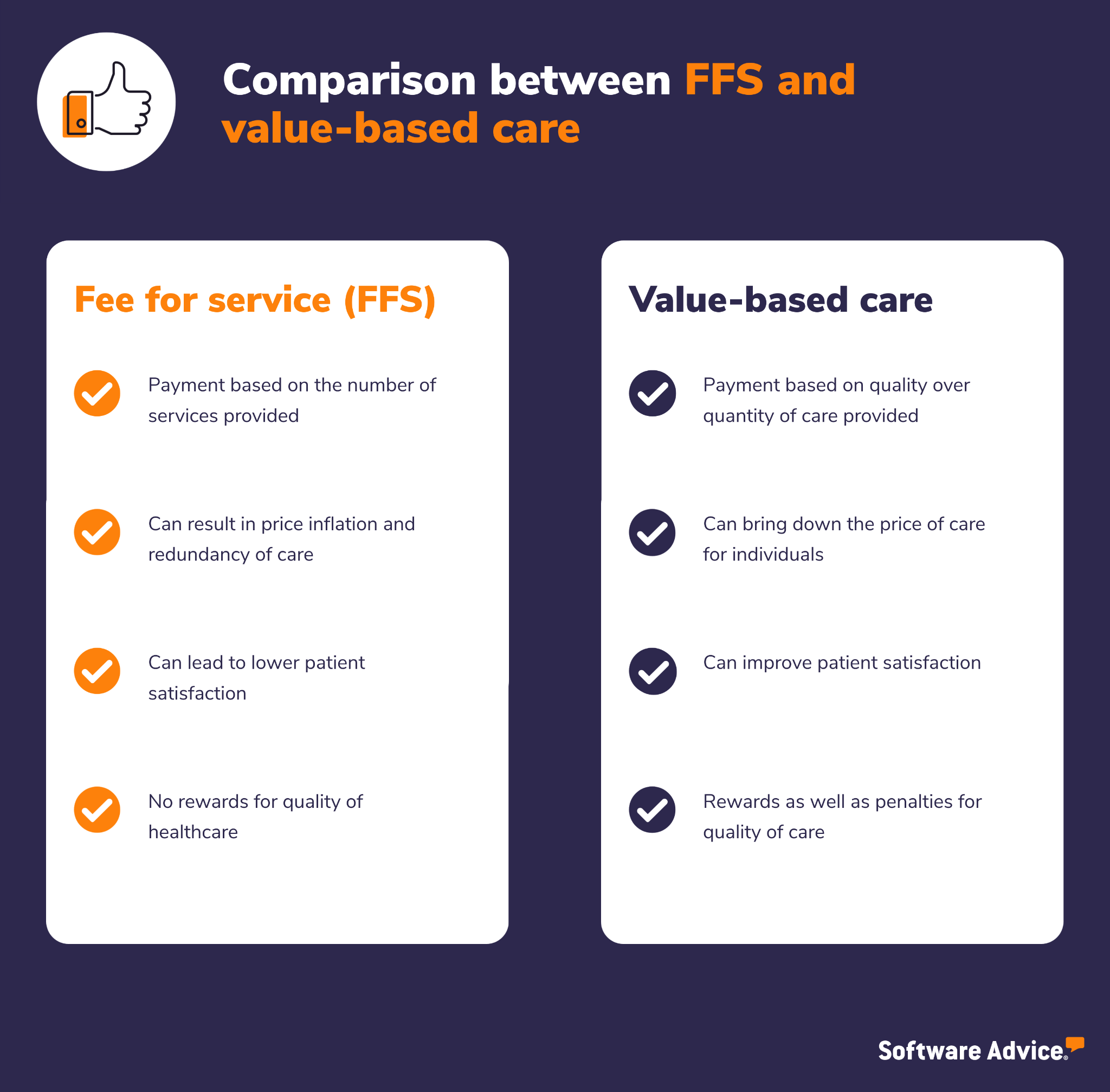
Comparison between FFS and value-based care models
What are the main types of value-based care models?
Let’s go over the two main types of value-based payment models available for a care provider or medical practice.
1. Accountable care organization (ACO)
An ACO is a network of doctors, hospitals, and other providers that works together to offer coordinated care to Medicare beneficiaries. ACOs aim to help practitioners ensure patients receive the right care at the right time as well as prevent redundant services.
Under this type of value-based care, network providers share in the savings if the ACO is able to provide adequate care and high-quality services that reduce healthcare costs for patients.
One potential downside—at least initially—is that providers assume some financial risk when joining. If the ACO provides excellent care and services, everyone shares in those cost savings, but if care quality isn’t adequate, providers in the network may have to repay Medicare for not delivering better care.
2. Bundled payments
Bundled payments allow patients to pay a single price for the services received during an entire episode of care, even if multiple providers have treated the same patient during an episode. The payment is bundled because all physicians, settings of care, and procedures are paid out together based on the treatment outcome.
For instance, if a patient has surgery, the Centers for Medicare & Medicaid Services (CMS) would pay the hospital, surgeon, and anesthesiologist bundled together based on historical prices instead of paying each separately.
Bundled payments have certain risks. If the providers in a bundled model are able to lower the cost of services below the bundled price, they can pocket the savings. But if the costs are more, they are responsible for the price difference.
Benefits of adopting a value-based care model
Let’s understand the key benefits of adopting a value-based healthcare model.

Benefits of adopting a value-based healthcare model
Patients spend less money for better healthcare
Value-based care doesn’t incentivize practitioners for throwing things at the wall to see if they stick. That means providers won’t benefit from recommending services their patients may not need or treatments that may not work, and that’s going to save patients money.
By encouraging practitioners to focus on providing personalized solutions to each patient’s underlying health issues, value-based care helps achieve better outcomes in the long run.
Providers are equipped to offer a better patient experience
A value-based model requires providers to be more efficient and strategic with the care they offer during each patient visit. It rewards them for delving deeper into the underlying problems patients may be experiencing instead of just running several tests, which can be costly, stressful, and uncomfortable for patients.
The doctor-patient experience is less transactional and more personal. During initial consultations, doctors and nurses spend time with their patients to get a more holistic idea about the reason for their visit. This improves the care experience for patients, as their needs are personally attended to.
Patients receive true value with their healthcare spending
Traditional FFS models incentivize doctor visits and prescriptions at their current prices, leading to inflated healthcare costs. Because of the high costs, many patients choose not to address their health issues until it’s too late or things have grown out of control, which becomes more costly in the long run.
By tying the cost of service directly to positive patient health outcomes, value-based healthcare helps lower the overall treatment cost for patients. It incentivizes doctors to be more thoughtful about what they prescribe and how they approach each patient. It also ensures physicians recommend only the most needed services, saving patients money on unnecessary tests or procedures.
Society is generally healthier
When healthcare costs are affordable, more people can access the quality care they deserve, which means they’ll be more likely to address chronic health issues earlier on.
Patients with chronic diseases are incentivized to care about their own health because they aren’t nervous about the financial risk. They’re more likely to seek help immediately and take control of managing their disease because they’re confident they have a personalized plan in place that is centered around their health and needs.
A value-based care model prioritizes patient satisfaction and experience and helps provide a more financially stable population that is able to address long-term illnesses with the best treatment methods available.
Value-based care is the future, and software can help your practice adapt
Value based care is becoming more and more popular because of the incentives the government is offering providers to make the change. With new legislation being passed, more providers are expected to make the shift and realize the benefits a value-based care model can give to their practice and patients.
One of the key challenges practitioners face is effectively tracking the metrics required to determine “value” in a value-based model. A healthcare organization will need to track staffing data, time and attendance of patients, clinical data, patient acuity data, and a bevy of other things to determine how to calculate cost of healthcare.
That’s where medical software comes into play. An electronic medical record (EMR) system, also known as an electronic health record system, can help your practice track and monitor patient health data from beginning to end.
Choosing the right software can be confusing and time-consuming. That’s where we come in!
Through one-on-one conversations and personalized recommendations, Software Advice guides you through your software search. In as little as 15 minutes, our software advisors can help you pick the right software for your business needs, so you can feel confident in your choice. Click here to chat with an advisor or schedule a call.