Ten Years of Technology: How the HITECH Act Influenced Physicians and EHR Adoption
It’s been 10 years since the HITECH Act passed, mandating the adoption of electronic health records (EHRs) in order to achieve “meaningful use.” After a decade of learning these new record systems, migrating data and dealing with support costs, many physicians are left with one big question: Was it worth it?
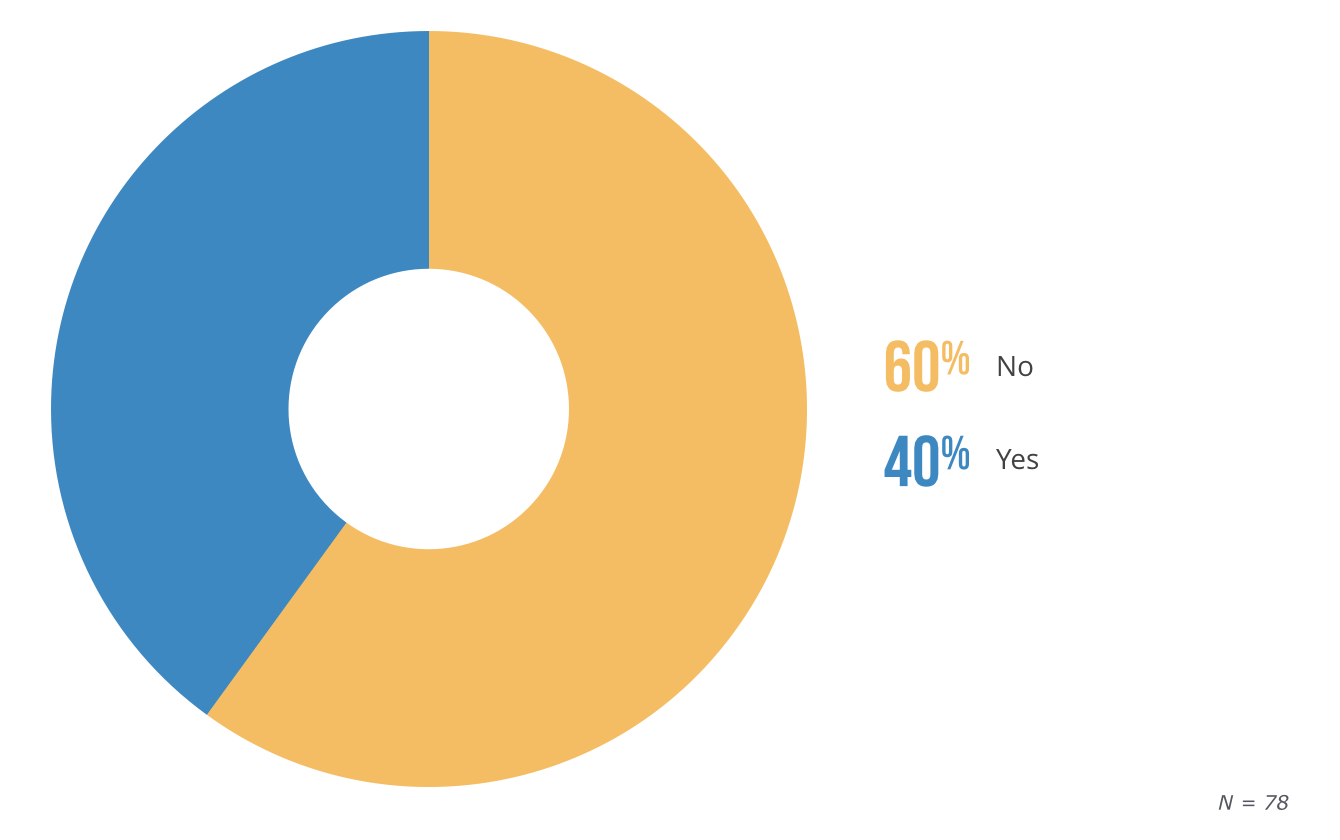
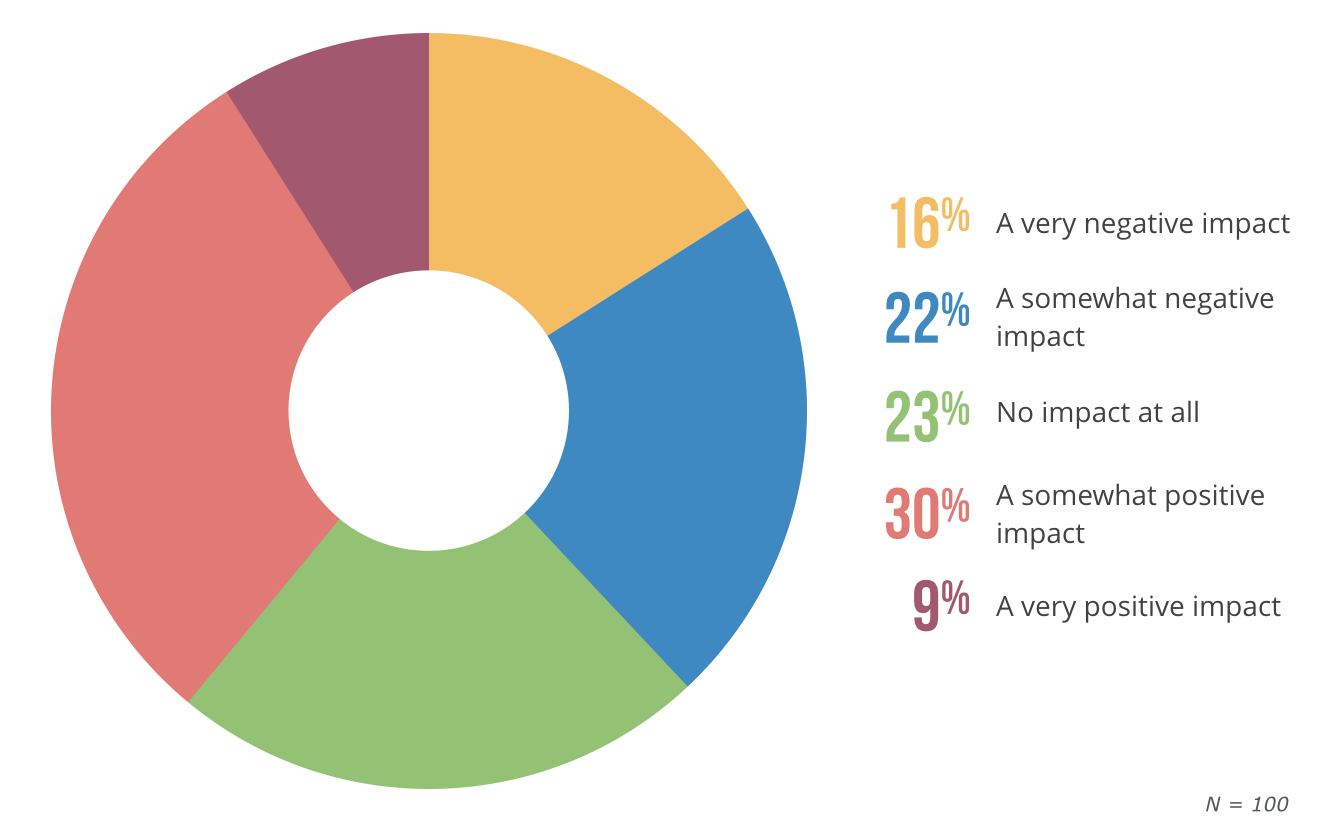
If you ask the doctors—which we did—you’ll get some mixed answers. For instance, when we asked the physicians in our survey whether or not the U.S. health care industry is generally better off today due to the HITECH Act, the majority said, “No.”
Is U.S. Health Care Better Off After the HITECH Act?
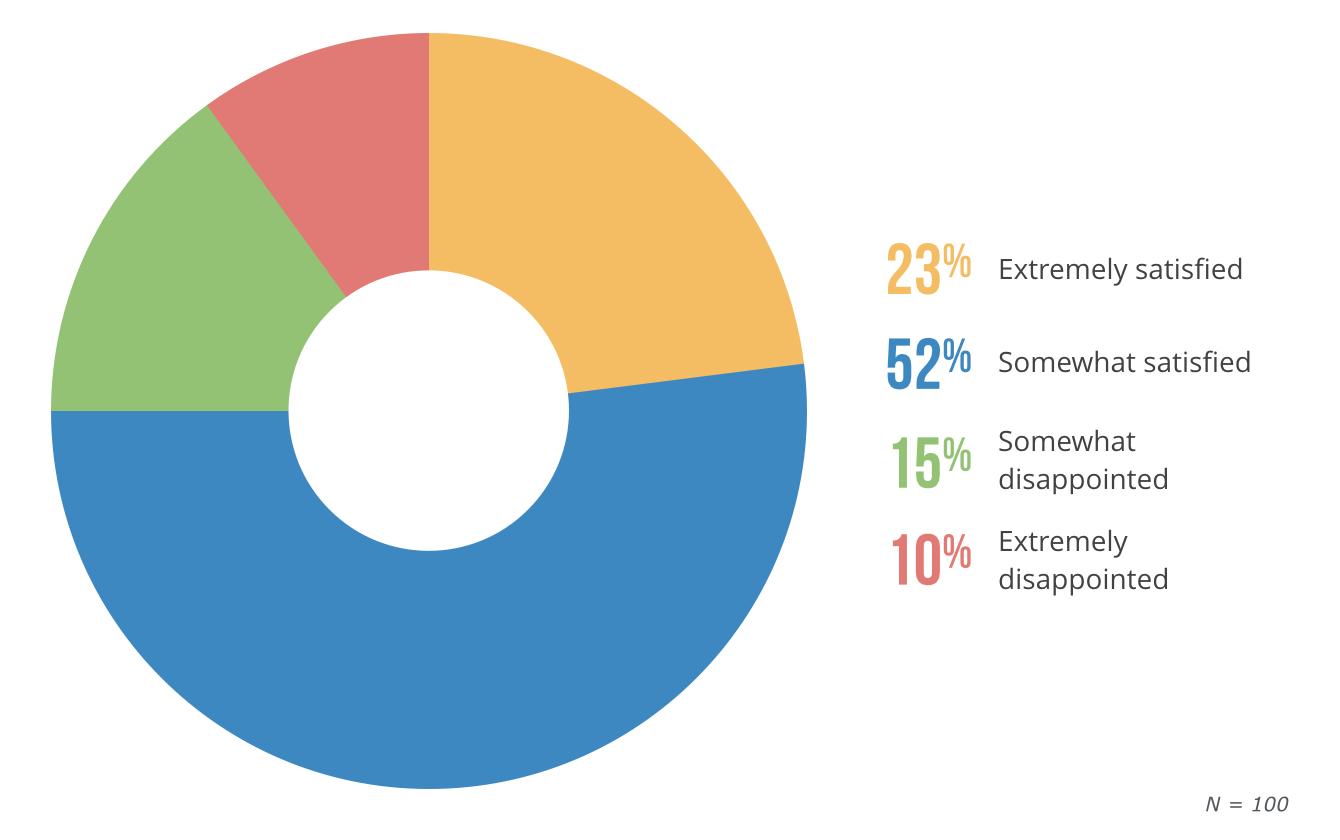
On the other hand, the majority of physicians we surveyed were satisfied with their EHRs, the adoption of which was a major priority for the HITECH Act.
So, how can so many physicians be so happy with their EHRs and still so disappointed in the HITECH Act?
In this article, we’ll break down the HITECH Act into more specific components and consider each of those smaller aspects’ effects on the day-to-day lives of physicians.
Here’s what we’ll cover:
Why Physicians Are Dissatisfied With HITECH, But Like Their EHRs
The HITECH Act Prompted Over Half of Physicians to Adopt EHRs
Physicians’ Expectations for the HITECH Act Didn’t Always Match Reality
Despite Overall Success, the HITECH Act Had Some Hits and Misses
Where the HITECH Act Succeeded, and Where There’s Still Work to Do
Why Physicians Are Dissatisfied With HITECH, But Like Their EHRs
When you consider the massive effort the HITECH Act represented, from the creation of the Health IT Policy Committee to the $19 billion set aside for grants to help train medical professionals on new IT, it might be a bit surprising that the majority of physicians we surveyed believe this legislation was detrimental to the U.S. health care industry.
What makes these results even more surprising is the fact that the HITECH Act’s primary goal was to increase EHR adoption among physicians—a goal that it absolutely achieved. And out of the same group of physicians in our survey, the majority reported satisfaction with their EHRs:
How Satisfied Are Physicians With Their EHRs?
To understand what accounts for this disparity, we have to break down the HITECH Act into more specific components and consider each of those smaller aspects’ effects on the day-to-day lives of physicians.
While the HITECH Act was flawed, it still achieved its most important goal, which was to drive widespread EHR use among physicians. But**, to realize the benefits the HITECH Act promised, physicians must fully embrace their EHRs and invest the time required to truly learn their electronic systems.**
HITECH Act History and Goals
The Health Information Technology for Economic and Clinical Health Act, aka the HITECH Act, was a piece of national legislation passed in 2009 as part of the larger American Recovery and Reinvestment Act (ARRA).
The highly summarized version is this: Government officials were seeing a lot of research that demonstrated how much technologies such as EHRs and clinical decision support could improve health care. They realized this would have massive implications for physicians, patients and protected health information (PHI). So they wrote a law to:
Encourage more physicians to adopt EHRs to ensure patient data would be more secure.
Expand protections for private patient data from security breaches.
Enhance penalties for HIPAA violations.
The HITECH Act created financial incentives for physicians who could demonstrate meaningful use of EHRs between 2011 and 2015, but those incentives turned into penalties for physicians who were still not using EHRs after 2015.
First and foremost, the HITECH Act wanted to increase the number of physicians in the U.S. using EHRs in a meaningful way. That last bit is crucial because it meant that doctors couldn’t just pay to switch to electronic records and be done with it. Instead, they had to use those EHRs to accomplish the other five goals of the HITECH Act:
Improve quality, safety and efficiency of care.
Engage patients in their care.
Increase coordination of care.
Improve health of the population.
Ensure privacy and security.
All of these goals are important, but we still have to make it through step one—getting physicians to switch to EHRs—before we can even start on any of the others.
The HITECH Act Prompted Over Half of Physicians to Adopt EHRs
Getting back to our physician survey, we asked our participants if the HITECH Act influenced their decision to switch from pen and paper methods to an EHR system. Turns out for most physicians, it did.
Did the HITECH Act Influence Your Decision to Switch to EHR?
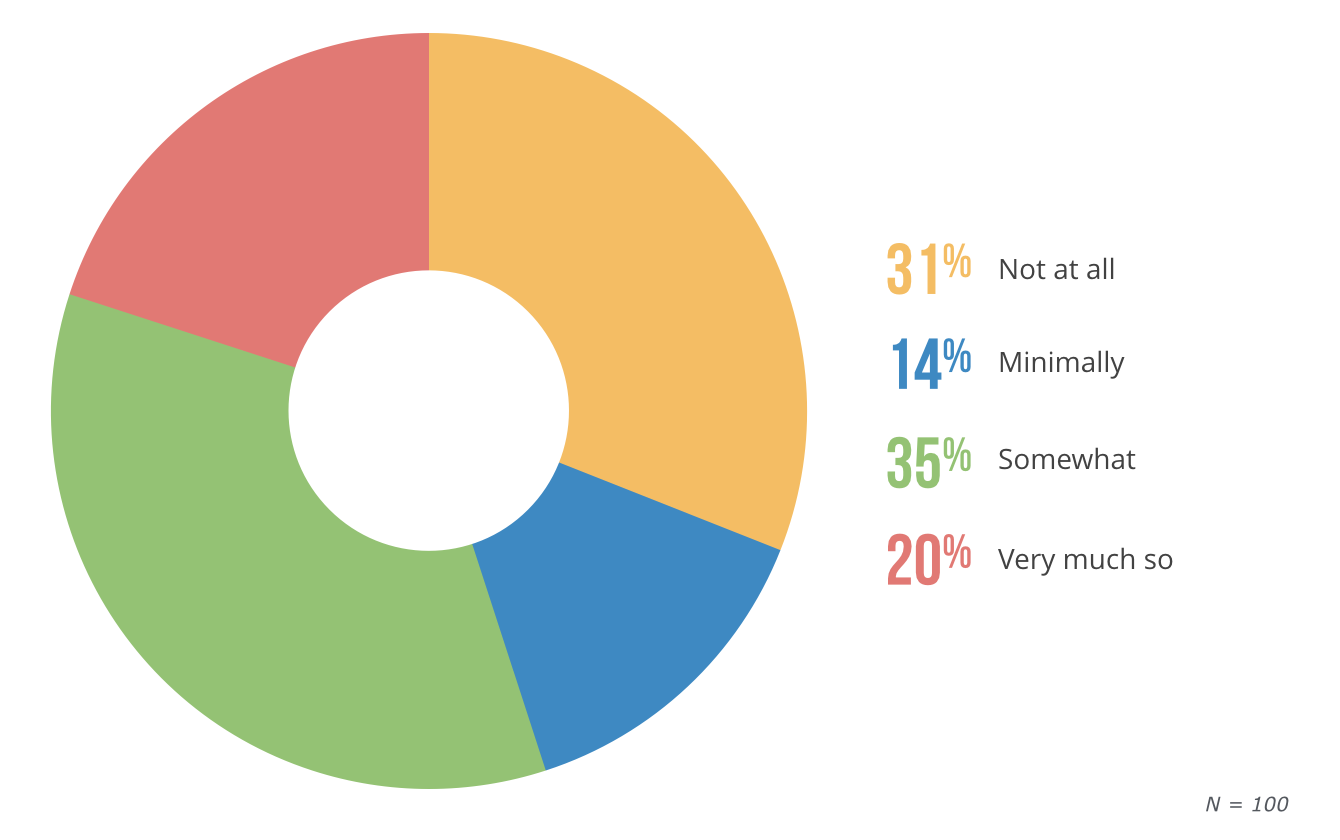
Here we have what I believe to be the single most impactful piece of evidence in support of the HITECH Act: Over half of physicians using EHRs are doing so because of the HITECH Act.
Had the HITECH Act not passed all those years ago, substantially more physicians would still be using old school pen and paper methods to track and store patient information.
Just by using ONC-certified EHRs, physicians are automatically taking advantage of so many security features designed to safely store, protect and share patient data.
That means complaints like the one left by one of our survey respondents that “Meaningful use is a joke—just useless tasks to be sure data is collected for accountants,” aren’t true at all. Simply using EHRs makes patient data safer.
For that reason, and because so many physicians only moved to EHRs because of the HITECH Act, it’s safe to say the biggest goal has been largely accomplished.
Physicians’ Expectations for the HITECH Act Didn’t Always Match Reality
In our survey, we asked physicians to think back to when the HITECH Act was first announced and describe how they expected it to impact the health care industry. We then asked physicians to describe how they felt the HITECH Act actually impacted the industry today, 10 years after it went into effect.
After removing the very small percentage of physicians who were not in practice when the HITECH Act was passed (5 percent), we found that the biggest change was from those who felt the law would have a somewhat positive impact to those who believe it had no impact at all.
Physicians' Expectations for HITECH Act's Impact in 2009
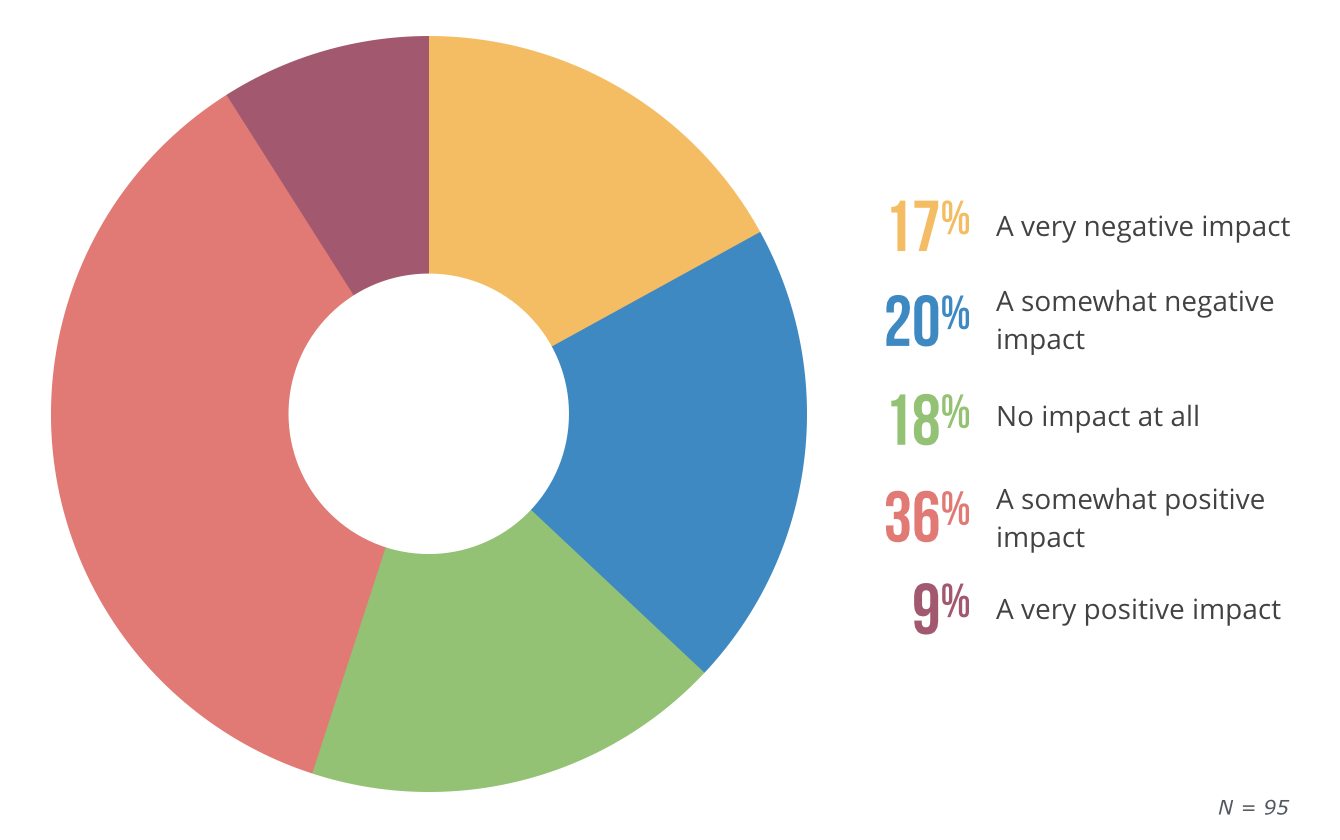
Physicians' Experience With HITECH Act's Impact in 2018
We asked our survey respondents to explain their answers in order to gain more insight, and we identified some revealing trends among those whose attitudes have changed over the past decade.
Trend 1: HITECH didn’t have a lasting impact
One physician who switched their answer from “a somewhat positive impact” to “no impact at all” originally expected the HITECH Act to lead to “improved legibility of records, better documentation, easier data collection and analytics,” but ultimately felt that wasn’t the case as they would have been using an EHR regardless of whether the HITECH Act incentivized it or not.
If you feel the same way as the above physician, that the legislation would result in advantages that you haven’t actually seen or would have seen regardless, I would ask you this: Could your expectations for the HITECH Act have been too high?
What our physician above is saying is, essentially, they had big expectations for the kinds of tangible benefits the HITECH Act would create. But since the major goal of the Act was to get more physicians to use EHRs meaningfully, it wasn’t actually trying to bring about those specific changes.
Instead, benefits such as “easier data collection and analytics” were meant to be more of a bonus for physicians who started using EHRs. Which, in fact, they were.
Trend 2: We’re not where we need to be
“I always dreamed about interchange health information with patients and facilities to reduce burdens of over utilizing resources,” but that dream has only “partially come true.”
In the same way as with the first trend, we had several physicians go from expecting “a very positive impact” to seeing only “a somewhat positive impact.”
In their expanded answers, the majority of those respondents talked about seeing a few of the things they were excited about when they first heard of the HITECH Act, but realizing that we still have a way to go before we’re enjoying the full list of benefits this technology could lead to.
Another physician in our survey had high hopes for accessibility thanks to the electronic platform, but has since found a “lack of interconnectivity” to be a disappointment.
To these physicians, I’d say you’re absolutely right. It’s true that a major motivator for passing the HITECH Act was the idea back in 2009 that, by providing secure and connected channels for exchanging information, electronic platforms could make health care so much easier and more efficient. And that’s something that hasn’t entirely been accomplished yet.
We’ll talk more about interoperability in the next section, but for now we can agree that the HITECH Act has at least set the stage for many of those future benefits by expanding the use of EHRs—and that’s a win.
Trend 3: EHR adoption has benefited patients and practices
“At the time, I thought it was a lot of hassle to be inputting everything in the computer. I also thought at the time that there was going to be a big learning curve as well as additional overhead costs in implementing the EHR.” But now, the same physician believes that “accessing medical records has never been easier or faster.”
Lastly, we took a look at some of the expanded answers for physicians who went from expecting “somewhat” or “very” negative impacts to actually seeing positive outcomes of the HITECH Act.
We found that many were initially afraid of the added costs, workload and training that an EHR would cause. One physician feared a slowdown in productivity, but has since found that their EHR is actually “good for documentation and legibility.”
One more respondent cited a common complaint among physicians that they were afraid the EHR “would be a divide between patient and doctor.” However, after learning to “type fast enough to keep up with most patients while talking to them,” they’ve come to appreciate the fact that “EMRs provide some checks and balances by screening decisions such as medication interactions,” a feature which greatly improves the patient experience, by the way.
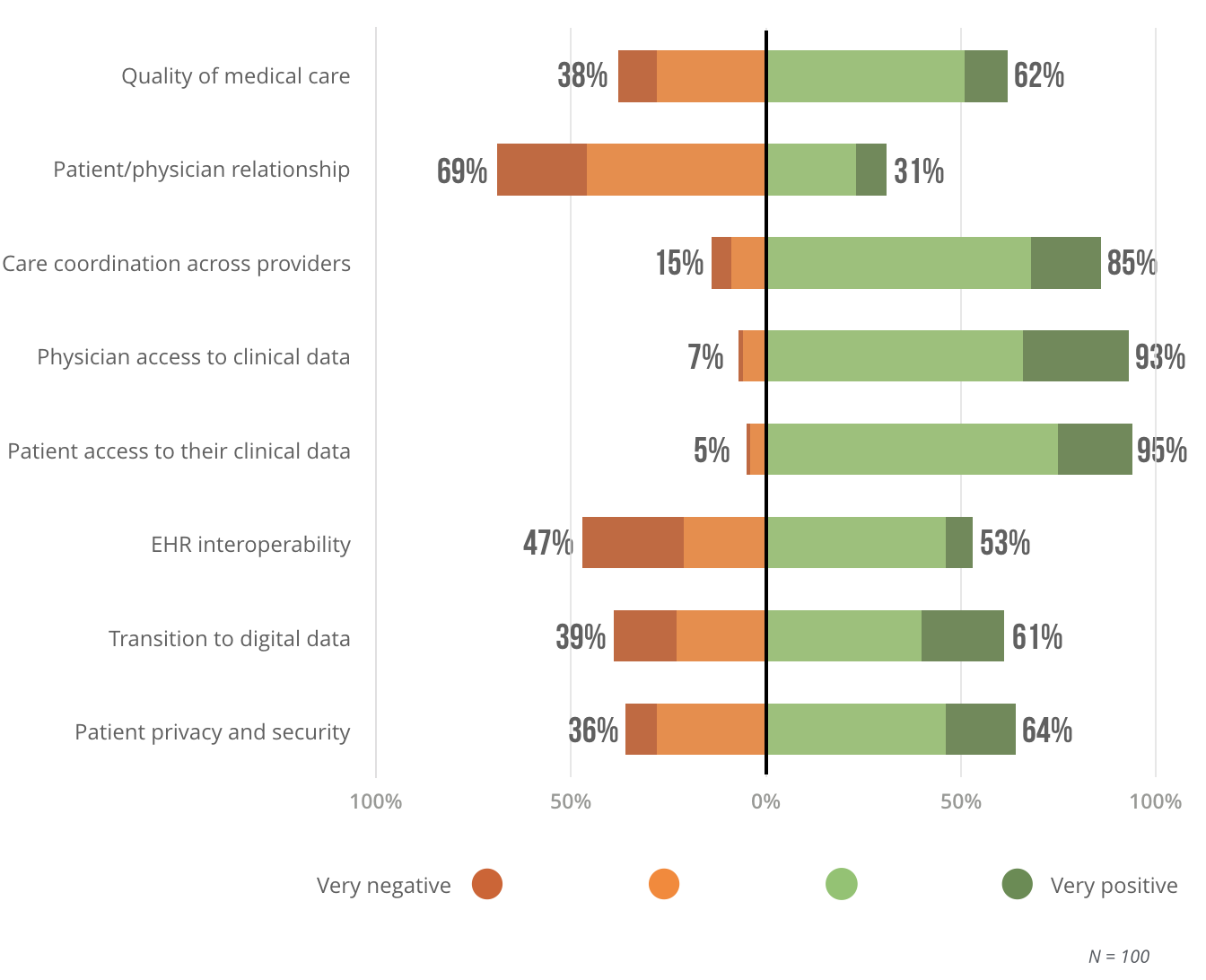
Despite Overall Success, the HITECH Act Had Some Hits and Misses
As great as it is that so many physicians are coming around to EHRs, the ones who still feel the Act wasn’t perfect have a point. We asked our physicians to describe the impact of the HITECH Act on eight specific areas of their practice, and while the results were highly varied, it’s apparent that, by and large, the Act has had a net positive effect on most of these things.
HITECH Act Impact on Small Practices
HITECH Hits
Let’s start with the really big wins since they’re more fun to talk about.
Patient access to their own clinical data. This is a big one. Patient portals have done wonders for improving patient engagement by making it so much easier to communicate with physicians, obtain and update medical information, view lab results, schedule appointments and fill out intake paperwork.
Also, features such as electronic referrals mean patients don’t have to deal with physical copies of their health records as much when seeing other doctors.
Bottom line: If you’re not already using a patient portal, you should start right away.
Physician access to clinical data/analytics. It stands to reason that the increased need to track and report in order to prove meaningful use would also result in an increased amount of clinical data collected, which physicians can then analyze in order to understand more about their own practices and make better decisions.
By keeping an eye on things like patient retention and attrition rates, patient satisfaction, financial reports, number of claims errors, physician referrals etc., physicians have a broader view of how their practice is doing as a business.
And now physicians can utilize practice analytics software to gain an even deeper understanding of what’s going on, which is always a good thing.
HITECH Misses
While it’s important to recognize that there’s more green on the above chart than there is red, it’s also obvious that they can’t all be winners. Still, I’m not surprised by the two biggest misses our respondents identified.
The patient/physician relationship. Remember our physician from above who was most afraid of EHRs interfering with the patient/physician relationship? That’s a very common issue among physicians, and it seems quite a few doctors are actually seeing that happen after adopting EHRs.
Using EHRs during exams can cause some distractions that may be detrimental to the patient relationship. If you’re looking at a screen instead of the person in front of you, or trying to find the exact code to fit your diagnosis instead of listening to your patient, you may not be providing optimal care. But that doesn’t have to be how you use your EHR.
There are plenty of solutions, many of which are incredibly easy to implement, that mitigate or solve these issues. Common solutions include:
Create workflows to make documentation simpler.
Rearrange your exam room so that your screen is in between you and your patient, making it easier to access information while interacting with the patient.
EHR interoperability. This is the biggest miss for the HITECH Act. Going back to our physician respondents’ expectations of HITECH, one put it well when they said they were initially excited by the prospect of “easier access to medical records,” but in reality it’s “not any easier to get information between doctors” today than it was 10 years ago.
Like I said, the HITECH Act has successfully accomplished step one of achieving widespread EHR interoperability, but there’s still a long way to go. What makes this issue more complex is the fact that it’s a bit of a chicken and egg scenario.
Take state HIE’s, for example. In order for these programs to be beneficial, many more practices—especially small practices—need to start participating. But most small practices aren’t ready to invest in EHRs with interoperability features until HIEs become more beneficial. It’s quite a conundrum.
That said, EHR interoperability is definitely on the horizon, and physicians should jump in sooner rather than later if they want to see this valuable health care network become a reality.
Where the HITECH Act Succeeded, and Where There’s Still Work to Do
To answer this question, let’s look at our list of “mini” goals to find out:
Increase EHR adoption and “meaningful use” among physicians: SUCCESS
Numerous studies have looked at the difference in EHR implementation rates before 2009 and after, and they’ve found that the HITECH Act has led to significantly more physicians using EHRs. Mission accomplished.
Improve quality, safety and efficiency of care: SUCCESS
Thanks to the widespread use of EHRs, doctors now have access to technology that assists with diagnosis by providing a broader view of patients’ medical history and reduces errors and risks, through features such as e-prescribing, with can identify potential drug interactions.
Engage patients in their care: SUCCESS
Just look at the results of our physician survey—95 percent of respondents said the HITECH Act had a positive impact on patients’ ability to access their own clinical data. It’s a cliche because it’s true: Patient engagement leads to better health outcomes.
When patients are actively involved in their care, they’ll take better care of themselves, be more honest and communicative with you and follow through on treatment plans. EHRs make all of these things easier for patients.
Increase coordination of care: PARTIAL SUCCESS
While the HITECH Act partially achieved this by laying the foundation for collaborative and coordinated care across different practices, the lack of widespread interoperability among EHRs shows that there is still a lot of work that needs to be done in this regard.
Improve overall health of the population: PARTIAL SUCCESS
While EHRs do make it easier to gather standardized information (such as immunization records and lab results) that can then be sent to public health officials for analysis, this seems to be one of the stickier requirements for a lot of physicians who resent having to track and report on so many different things.
This sort of meaningful use is still seen as a burden by most doctors, so despite widespread EHR use, there’s more work to be done before it can be said EHRs are improving health outcomes for the entire population.
Ensure privacy and security: SUCCESS
The HITECH Act’s mandate that physicians must be subject to audits that help determine HIPAA compliance has greatly improved the privacy of patient data. Since EHRs are built with security features designed to make patient data more secure, physicians are accomplishing this goal simply by using EHRs.
So there you go. Four out of six goals completely accomplished, and the other two are well underway. Was the HITECH Act worth all the hassle of buying EHRs, figuring out how to use them, transfering all your patient data and spending more time on notes and reports?
Yes. Absolutely.
Here’s how I know: Physicians who took the time to switch to EHRs in the early days of the HITECH Act—back when they were still being incentivized rather than penalized—are far ahead of physicians who resisted the change.
They’re seeing the benefits to their practices and their patients, and are also much better positioned for future developments such as the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the transition to value-based care.
If you’re one of the physicians still struggling with your EHR, your only real option is to stop resisting the change. Instead, fully embrace the transition to electronic methods and take the time to train and learn shortcuts so you can get the absolute most out of your EHR. All evidence points to EHRs being the future of medicine, so there’s really no point fighting it.
Demographics
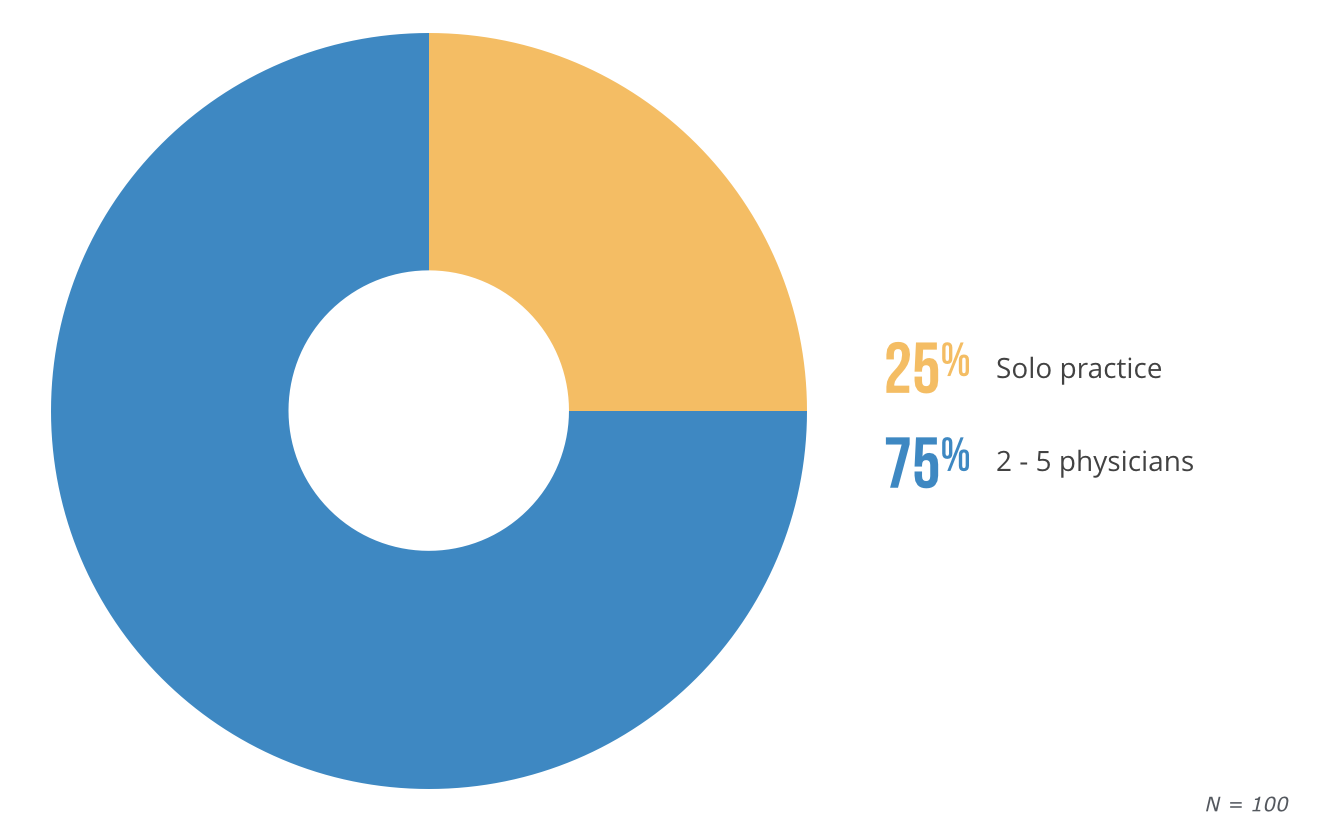
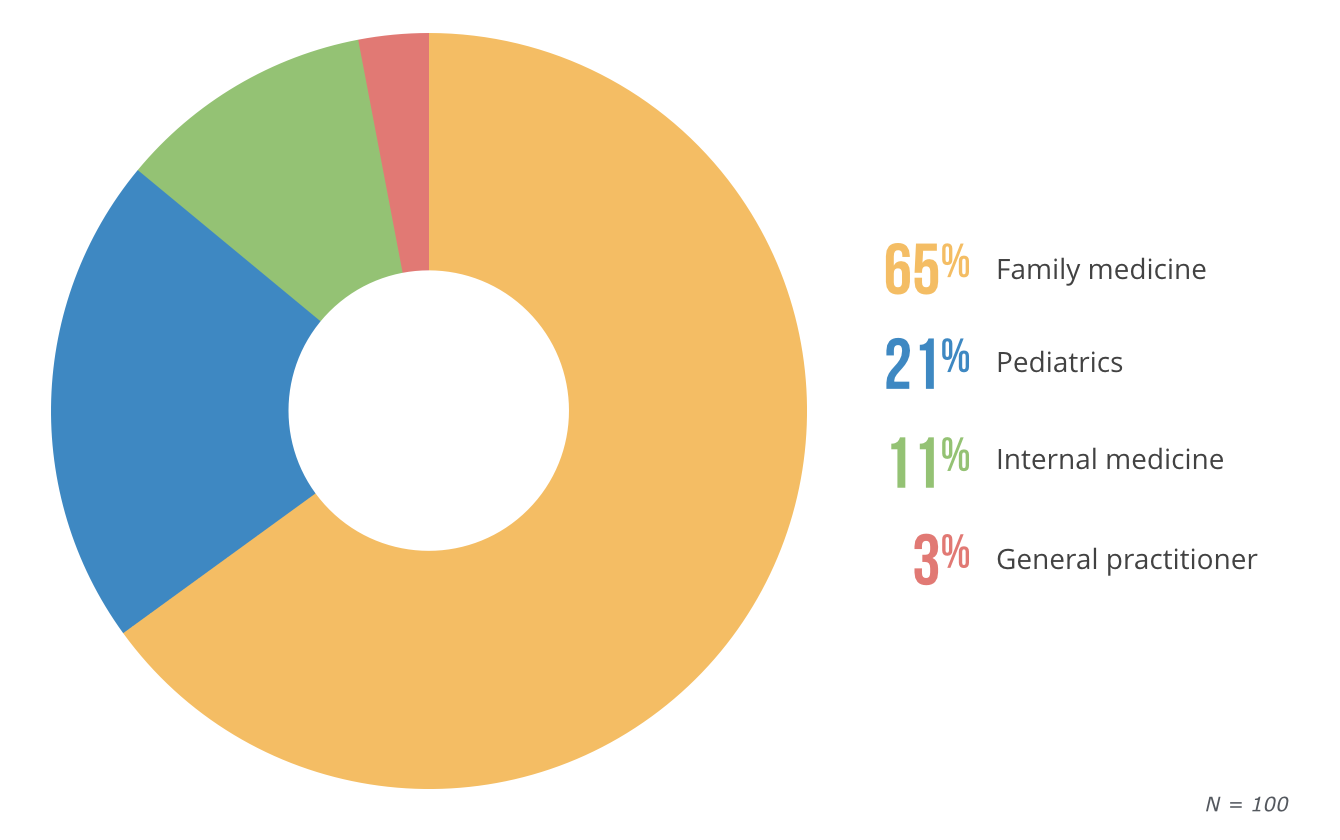
We partnered with SERMO to conduct our survey of 100 U.S. physicians working at small practices (defined as five or fewer physicians) with few to no specialty-specific EHR requirements.
The demographics of our survey respondents broke down to 25 percent solo practices and 75 percent of practices with between two and five physicians. The majority of physicians in our survey (65 percent) specialize in family medicine, with pediatrics and internal medicine following at 21 percent and 11 percent, respectively.
Size of Practice
Type of Practice
If you have comments or would like to obtain access to any of the charts above, please contact lisa@softwareadvice.com.