What Is Big Data in Healthcare, and How Is It Already Being Used?
Understanding what kinds of gains the healthcare industry is making by using big data analytics is crucial for you to better care for your patient population. After all, knowing where to upskill or invest in new resources to use data more effectively can improve your patients’ outcomes.
While it might not be attainable for small practice owners or admins to access the AI-powered tools larger healthcare organizations use to analyze their healthcare data, it’s important to understand the types of benefits that come with that data analysis in order to adjust your best practices.
To that end, we’ve leveraged Gartner insights[1] to give you information about big data that you need to know. Additionally, we’ll go over what big data in healthcare is and why it’s crucial that you gain familiarity with it in order to improve your practice.
What is big data in healthcare?
Big data in healthcare refers to the vast quantities of data too large or complex for traditional technology to make sense of. This data was and is created by the mass adoption of the Internet and digitization of all sorts of information, including health records. It’s not just quantity though; it’s also velocity and variety. Essentially, it’s the vast amount of different data that is coming in at a speed in which a human cannot possibly interpret.
The types of data gathered can range, but since the wide-span implementation and adoption of electronic health records (EHR) software, hospitals and healthcare organizations have greater access to all of their patients’ data in a digital, scannable format. Big data includes:
Medical records
Dental records
Surgical records
Behavioral data (such as a patient’s diet or level of physical activity)
Biometrics (such as a patient’s blood pressure)
Living conditions
It’s not only healthcare data either. You can analyze non-healthcare data as well if you utilize any of the following patient engagement methods:
Social media engagement
Marketing efforts
Patient experience (patient portal usage, patient retention, etc.)
Satisfaction via patient satisfaction surveys
You can even gain insights by tracking other forms of healthcare delivery data:
Staffing schedules (you might find that you only need X members of staff to be on call during X hours)
Patient waiting room times
Insurance claim data
Medical referrals
Employee performance metrics (such as the number of patients seen each hour)
Supply chain metrics (such as making sure you’re ordering the proper amount of testing equipment or PPE)
This isn’t even all of the available data points you have access to. The point is, if you’re not considering and using at least some of these data points to drive decision-making, you’re leaving a lot on the table. It’s a matter of figuring out which are the most important for you.
Additionally, the problem has traditionally been figuring out how to collect all that data and quickly analyze it to produce actionable insights. But with emerging big data technologies, healthcare organizations are able to consolidate and analyze these digital treasure troves in order to discover trends, better treat patients, and make more accurate predictions.
It's worth noting that smaller practices might have the quantity of data, but that data might not necessarily be coming in at a speed which would necessitate an investment into big data tools to properly analyze. If that’s the case, it’s still important to have a handle on the data that’s incoming so that you can analyze it in order to improve decision-making.
Big data in healthcare is a major reason for the new MACRA requirements around EHRs and the legislative push toward interoperability.
Why do you need to care about big data in healthcare?
All of this data is coming into your practice, and if it’s just sitting there without being used, you’re missing out on insights that could help you correct mistakes or improve on your processes to make them more efficient.
Analyzing and using the data your practice gathers is essential to growing your practice as well as gleaning insights into how you can improve patient outcomes or get better ROI with marketing efforts.
That said, there are several factors to consider whenever you think about how big data can improve your practice:
Even healthcare organizations with advanced data science capabilities struggle with people and process barriers to delivering value at scale or improving data-driven decision-making.
Healthcare data can be extremely complex and fragmented across hundreds of information systems.
Complex healthcare problems do not necessarily need large investments or complex data science solutions to generate value.
There’s an inherent human lack of trust in advanced analytics, especially when the models are used to predict critical clinical decisions, and an inability to ensure ethical use of data and analytics.[1]
That’s why practice owners must ask themselves a few things before investing in big data tools:
“How can we treat data as an asset?”
“With this data or this type of insight, how can we improve clinical outcomes for patients?”
“How can we use data to advance value in our healthcare organization (e.g., improved health, managed medical costs, positive experiences for patients and clinicians)?”
Why you must treat data as an asset
Whether or not you make the plunge and invest in the staffing and technological improvements necessary to utilize all of the data coming through your practice, you must still treat data as an asset.
By analyzing the available data coming into your practice, you can identify gaps you might have when it comes to patient care, patient outcomes, or even staffing decisions. Utilizing the data as an asset can dramatically improve the accuracy and timeliness of predictions for patient outcomes, which reduces costs, improves care, and saves lives.
For example, practice owners who draw from big data samples might be able to identify warning signs of serious illnesses in their patients before they arise which means treating that disease at an earlier stage. This can lead to better health outcomes for the patient as well as cheaper care in the long run because they can better manage symptoms.
Additionally, administrators can use data to make funding and resource allocation decisions. By analyzing the staffing data you have, you can determine how best to allocate your staff and resources. For instance, if, by analyzing the data, you find that you consistently have a spike in emergencies from 11:30 AM to 3:30 PM, you might want to have a few extra members of staff on that shift.
This not only helps you save money by reducing unnecessary staffing when it might be relevant, but it also helps increase patient satisfaction because you’re never understaffed during busy hours. It might also help save lives.
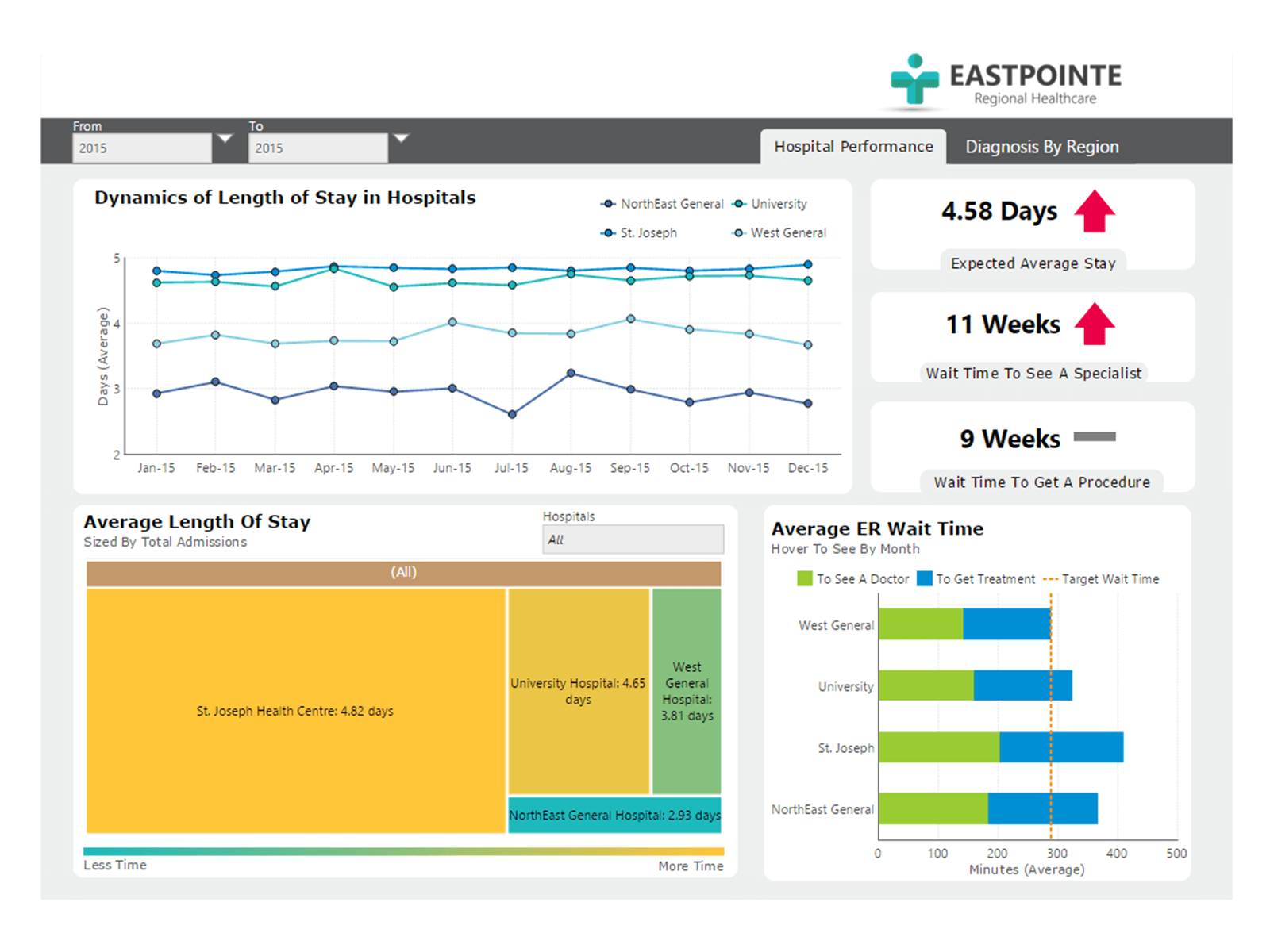
An example of what kinds of administrative data can be gathered (Source)
However, despite conventional wisdom, simply adding data does not lead directly to organizations making better decisions. You’ll need to explore, investigate, and supplement your thinking with the experience and knowledge you’ve gained from your time practicing, and bring all these bits of information together into a scheme for making data-driven decisions.
Small practice applications: Even if you aren’t going to spring for the most sophisticated big data analytics tools, if you’re a small practice owner or administrator, you need to better utilize the data you’re accumulating if you want to not only stay competitive, but also improve patient outcomes.
The types of insights you can glean in order to improve clinical outcomes for patients
Understanding the big picture of big data in medicine is important, but so is recognizing the real-world applications of data analytics as they’re being used today.
To that end, here are a few notable examples of big data analytics being deployed in the healthcare community right now.
More accurate diagnoses
Right now, data analytics tools exist that provide better clinical support, at-risk patient population management, and cost of care measurement. Many of these systems have established expansive databases—some with billions of data points—that they can then apply sorting and filtering algorithms to in order to rapidly analyze all that information.
These systems allow users to pinpoint how variations among patients and treatments influence health outcomes. Based on these insights, providers can determine more precise treatment plans for individual patients or patient populations. For example, you can analyze check-up results among your patients in different demographic groups in order to identify what factors might discourage people from taking up the treatment you recommend.[3]
Small practice applications: Small practice owners can benefit from these data points by investing in big data tools in order to gain access to the bevvy of analytics that already exist out there. You can cross check your patient population with the data that’s already available to help improve decision-making.
Predictive medicine
Genomics is the next frontier of medicine. The cost of genome sequencing is falling—you can sequence your complete genome for a couple thousand dollars these days, down from around $100 million a decade ago. As a result, the volume of genomics data is growing rapidly—and so is our ability to take advantage of that data.
Using genomic data is one way we’re already able to more accurately predict how illnesses, such as cancer, will progress.
For example, Emory University and the Aflac Cancer Center partnered with a genomic data analytics organization called NextBio to study data related to medulloblastoma, the most common malignant brain tumor among children.
Medulloblastoma currently has a uniform treatment approach: radiation therapy. Emory and Aflac are using NextBio to look at clinical and genomic data to discover biomarkers that can help predict the metastases of cancer in young patients. Providers, in turn, will use this information to pinpoint targeted therapy approaches based on the biomarkers of their individual patients.[3]
Small practice applications: While it might not necessarily be super achievable for small practices to partner with labs that do genome sequencing, it’s important to stay abreast of the developments and outcomes that these technologies and studies are finding so that you can use them in your practice.
Population health management
While big data’s main goal for medicine is to improve patient outcomes, another major benefit to data analytics is cost savings.
For example, Dr. Ghassan Salman of Texas-based Austin Diagnostic Clinic[2], uses his EHR data to "identify groups of patients with gaps in their care."
He says a program within their EHR can quickly spot patients in need of breast cancer screenings by analyzing specific patient populations, their names, their last date of service, and the results of their last mammograms.
Some systems are able to collect information from revenue cycle software and billing systems to aggregate cost-related data and identify areas for reduction.
The University of Florida made use of Google Maps and free public health data to prepare heat maps targeted at multiple issues, such as population growth and chronic diseases. Subsequently, academics compared this data with the availability of medical services in most heated areas. The insights gleaned from this allowed them to review their delivery strategy and add more care units to the most problematic areas.[4]
Small practice applications: As demonstrated by Dr. Salman’s example above, small practices already have access to population health management data if they utilize the data already acquired in their EHRs. Additionally, it’s important to stay on top of research being conducted that can help practice owners better understand their population health management.
Enhancing patient engagement through wearables
Many of your patients are already readily engaging in data gathering by wearing smart devices that record every step they take, their heart rates, or sleeping habits on a daily basis. This is all vital information for healthcare professionals that can be coupled with other trackable data in EHRs to identify any lurking health risks.
For instance, chronic insomnia and elevated heart rates might signal a risk of future heart disease.
In our 2022 Software Advice Patient Wearable Survey [*], we asked patients what the biggest benefits of their wearable technology are, and the number one response was that it gives them a better understanding of their own health.
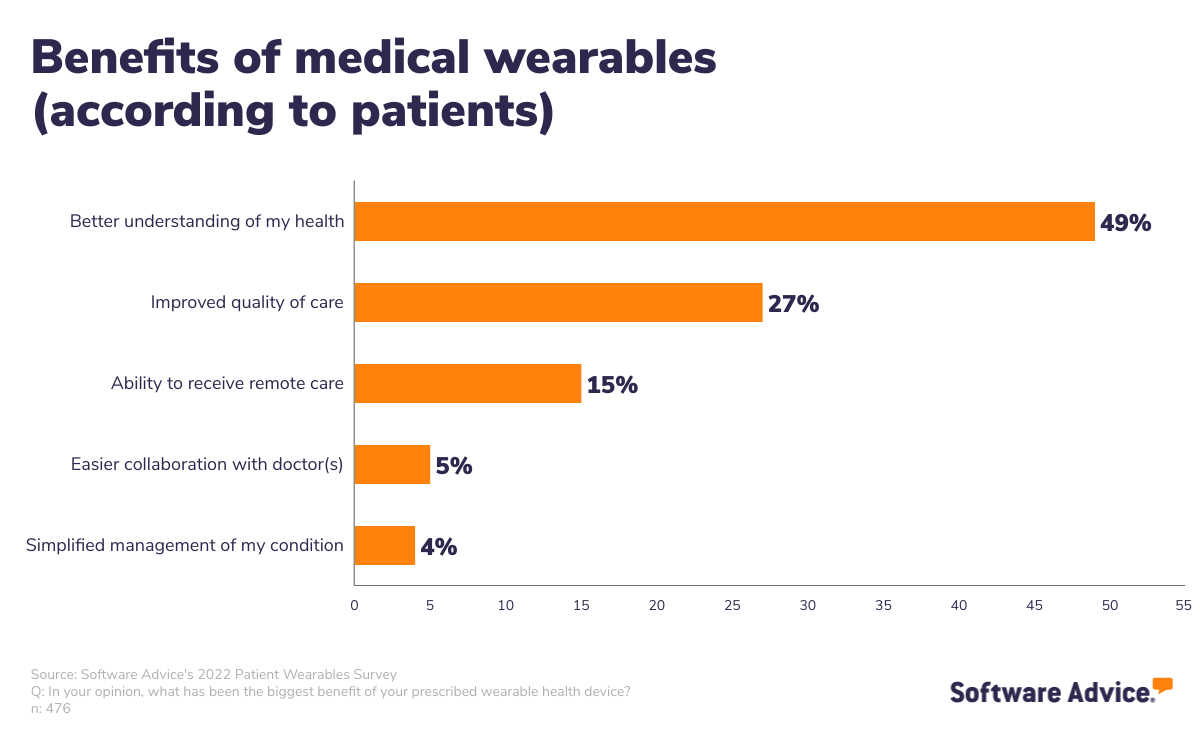
In addition, that same survey found that 86% of patients agreed that their wearable do all of the following:
Enables doctors to provide a higher quality of care
Improves their health
Improves their quality of life
It’s not just smart watches that can gather meaningful data. Remote patient monitoring (RPM) devices have become more and more critical in developing effective long-term strategies to manage and treat chronic care conditions. Remote monitoring devices have been used in healthcare for a while, but advancements in technology have made them “smart.”
Pulse oximeters can help patients with asthma and other lung or heart problems.
Continuous glucose monitors help patients with diabetes understand what factors affect their chronic condition.
Blood pressure cuffs help patients with high blood pressure monitor their condition.
All of these devices upload their data via the cloud into your systems, which can help you spot potentially concerning trends. You’ll be able to see where spikes occur, and having access to all of this data ahead of appointments allows you to think critically about the trends instead of wasting time during the office visit to look at the results they would traditionally have to bring to you manually.
Small practice applications: Small practice owners can have great success improving patient engagement by asking for and implementing smart device data into their care management. Patients are already interested and using this data to inform their own health decisions, so it’s a win-win to incorporate it yourself. Additionally, RPM should be considered if your patient population consists of a large number of patients suffering from chronic conditions such as diabetes, heart disease, or asthma.
What small practices need to know about big data
So, this is all well and good for major health organizations that can afford big data analytics tools today, but what does this mean for the smaller, independent practice?
Complex business problems do not necessarily need large investments or complex data science to generate value. As long as your practice develops key principles and processes to follow whenever analyzing data, you’ll be in good shape. You want to take the time to check assumptions and experiment to increase value. The faster you can utilize your data, the faster you can improve health quality and outcomes, coordinate healthcare services, and, ultimately, decrease the total cost of care for your patients.[1]
Additionally, legislators have been talking about empowering medical providers to become more connected for a long time, but only recently has interoperability truly become imperative for Medicare reimbursement qualification. MACRA is now incentivizing interoperability and requiring the use of EHRs that support interoperable functionality.
Small practices can often struggle with MACRA regulations because it can be difficult to measure value unless you have the necessary technology, which can be expensive. That said, the increases in interoperability go a long way toward improving the ability to track and measure value because you have more access to healthcare data across different practices. In addition, small practices can voluntarily join a Virtual Group[5] to participate in the Merit-based Incentive Payment System (MIPS).
For more information about how interoperability is helping healthcare providers, check out Interoperability in Healthcare: A Guide for Small Practices Choosing Software.
Outside of federal regulations, investors also see big data as a huge moneymaker—and more investment will lead to more solutions.
Big data in healthcare is here to stay, so learn to utilize it
Now that you have a greater understanding of what big data in healthcare is and how you can utilize some of the gains gathered by larger healthcare organizations, you’re ready to determine whether or not you need to invest in the tools and services necessary to implement it effectively.
You might think about investing in a data analytics expert full time in order to better understand the data you’re already collecting. You might also choose to invest in more sophisticated software:
At the very least, you should be utilizing the data you’ve already collected via your EHR and other tools to drive decision-making and improve health outcomes for your patient population.
Note
As you continue to uplevel the way you collect, review, and apply patient data, it’s important to prioritize training and security to avoid being one of the 36% of healthcare organizations in the US that have experienced a data breach [**]. Read more about how to avoid this here: More Than a Third of Medical Practices Have Experienced a Data Breach—49% Were Caused by Human Error.
And, as always, if you’re looking to improve your software stack by investing in new technology, our advisors are always here to help.
Through one-on-one conversation and personalized recommendations, Software Advice guides you through your software search. In as little as 15 minutes, our software advisors can help you pick the right software for your business needs, so you can feel confident in your choice. Click here to chat with an advisor or schedule a call.
Sources
CDAO Industry Review: 6 Case Studies for Building a Data-Driven Healthcare Organization, Gartner
Dr. Ghassan Salman's LinkedIn Page, LinkedIn
NextBio Teams With Emory University and the Aflac Cancer Center to Improve Outcomes for Children with Medulloblastoma, PR Newswire
Neighborhood-Level Hot Spot Maps to Inform Delivery of Primary Care and Allocation of Social Resources, National Library of Medicine
Virtual Group Participation, Center for Medicare Services
Survey methodology
[*] Software Advice conducted this survey in January 2022. We used screening questions to narrow respondents down to 476 living in the U.S. with relevant medical experiences and knowledge, including diagnosed chronic conditions currently being treated or managed with medically prescribed wearable devices.
[**] Software Advice conducted this survey in February 2022 of 259 healthcare providers. We used screening questions to narrow the respondents down to those who currently work at U.S. practices and are at least partially responsible for IT management and/or data security.
We divided our respondents into small and large practices according to the number of licensed healthcare providers currently working there. Small practices have one to five providers; large practices have six or more providers.