9 Must-Have Medical Software Features for Small Medical Practices
There are hundreds of medical software solutions available on the market, and their functionalities and price vary widely, depending on the vendor. Searching for the right medical software takes valuable time and resources away from focusing on patient care and timely reimbursement.
A checklist can really help small practices identify what features and tools they’ll need along their journey.
 Through this article we’ll help you navigate the medical software market, understand the features you may need, and invest in different types of healthcare IT during your practice’s growth.
Through this article we’ll help you navigate the medical software market, understand the features you may need, and invest in different types of healthcare IT during your practice’s growth.
We’ll break down what technology a medical service provider needs to start with, grow its capabilities over time, and optimize operations down the line.
While this guide targets small and independent practices, it can be a helpful resource for any medical professional.
Here’s what we’ll cover:
Needs Cycle for Small Medical Practices [GRAPHIC]
3. Billing
Healthcare IT to help you grow
Healthcare IT for optimization
7. Telemedicine
9. Patient relationship management
We’ve consulted primary sources, including actual medical software buyers from small practices, as well as secondary sources to create this Medical Software Needs Cycle. Read our detailed methodology at the bottom of the page.
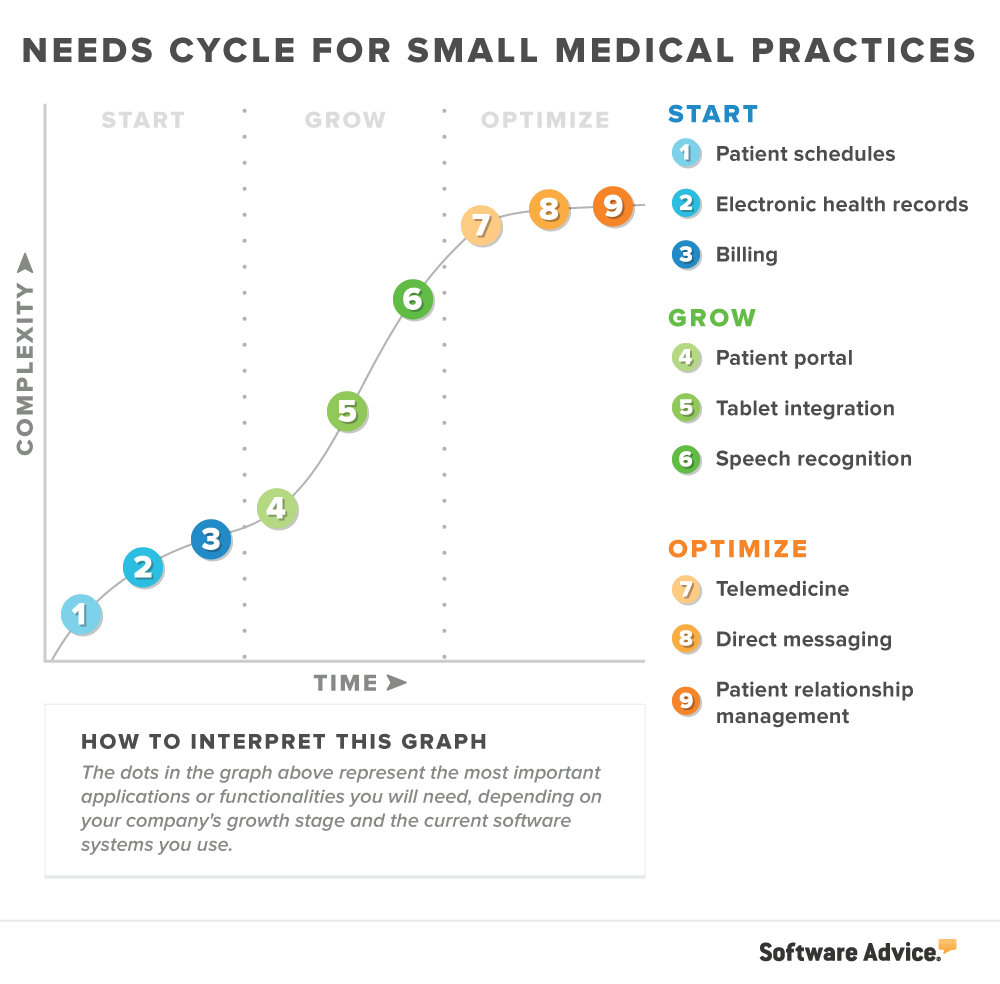
Healthcare IT to start with
This section is for medical practices that are about to start operations and need basic software (with core features) to handle daily tasks.
1. Patient scheduling
What it is: Scheduling software helps you set and manage patient appointments. You enter into it patients’ contact information, demographics, appointment time, chief complaints, and billing information.
See examples of patient scheduling software and read more detailed descriptions in our Buyers Guide.
Why you need it: While you can set reminders on Microsoft Outlook and earmark appointments on Google Calendar, these tools aren’t HIPAA compliant and would consume a lot of time. Also, they can’t accommodate the depth and breadth of patient information you’d need during patient visits.
Patient scheduling is first on our Needs Cycle for a reason. We found it topping the list of the most requested applications (based on inquiries by 4,200 medical software buyers):

Key considerations:
A lot of electronic health records (EHR) software includes some scheduling capabilities, so hold off on buying a standalone scheduling system if you’re also shopping for an EHR.
To reap maximum benefits from scheduling technology, consider systems that send automated phone, email, or text message reminders to patients. These features may cost extra, but they’re popular with medical practices as a means of preventing no-shows.
2. Electronic health records (EHR)
What it is: Electronic health records (EHRs) provide digital storage of patient health data and include functionalities to track patient demographics, medical history, SOAP notes, medications, test results, and more.
See examples of EHR software and read more detailed descriptions in our Buyers Guide.
Why you need it: Use of EHR software plays a major role in qualifying for government incentives awarded by certain regulations (MACRA, MIPS, etc.) for healthcare IT adoption.
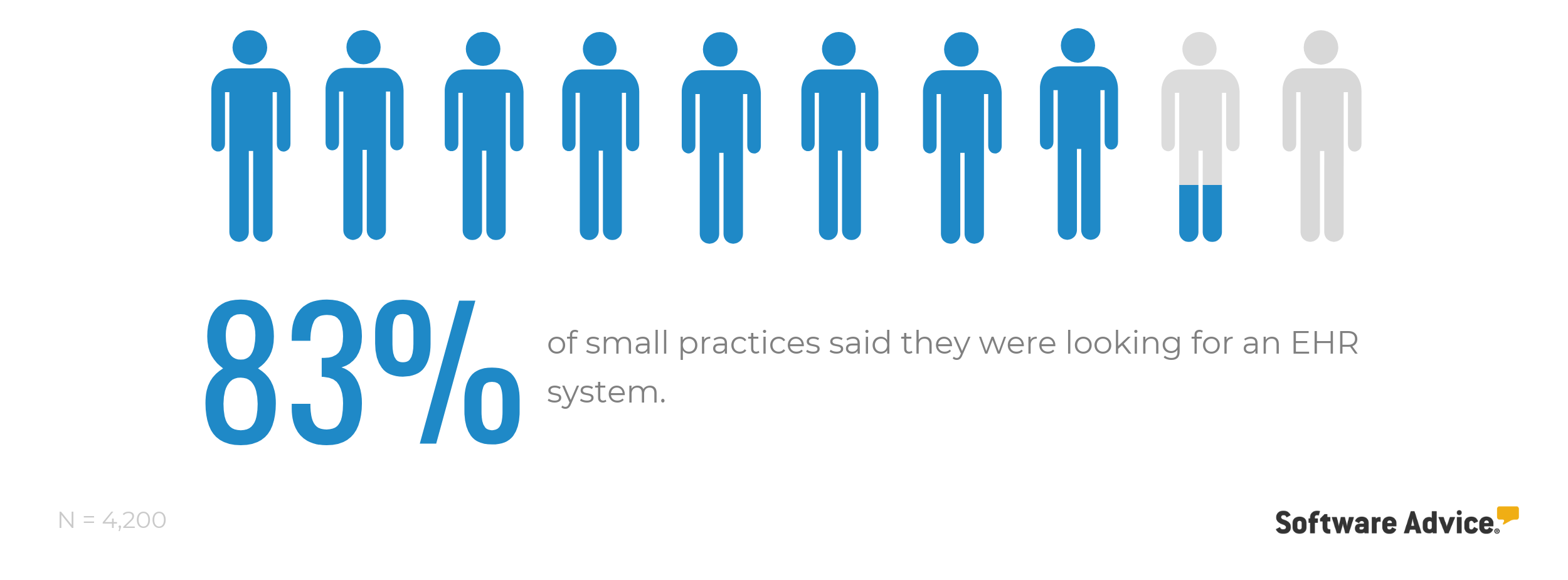
That said, government mandates aren’t the only reason you need an EHR. The benefits of these systems include greater data accessibility, improved clinical reporting, and greater care coordination. In our study of medical software buyers, eight out of 10 practitioners told us they want an EHR:
Key considerations:
Opt for an ONC-ATCB-certified EHR that meets capability standards set by the government, such as ensuring that the system offers e-prescribing functions.
You should also look for systems with integrated population health tools, such as care path enablement and gaps-in-care reporting. These tools will become increasingly important as healthcare payment models shift from volume of services rendered to value of treatment.
To derive data trends specific to your practice, look for EHR systems that include reporting and analytics tools. These functionalities would help you understand how your practice is operating and how it can improve.
3. Billing
What it is: Medical billing systems help providers generate patient bills, manage collections, and create financial reports. They also automate the process of coding, submitting, and tracking claims.
See examples of billing software and read more detailed descriptions in our Buyers Guide.
Why you need it: You got into healthcare to help people—not to agonize over rejected claims and complicated ICD-11 codes. Using billing software is like having a digital assistant that ensures that your claims are accurate and provides data-driven insights into your practice’s financial health.
About three-quarters of the small practices we spoke with expressed interest in buying billing software.

The only circumstance wherein you wouldn’t need a dedicated billing software is when you’re outsourcing billing operations, which takes away a percentage of your collections. Find out whether you should be outsourcing your billing here.* Medical practices typically do not need a separate accounting solution, since medical billing systems handle patient accounts, posting payments, printing statements, and running ledger reports.
Healthcare IT to help you grow
This section is for practices looking to save time and increase revenue by leveraging mobile devices and patient-facing technology.
4. Patient portal
What it is: These secure tools give patients anytime access to messages, services, and information related to your practice. That includes the ability to review medical records, pay bills, book appointments, and request medication refills.
See examples of _patient portal software and read more detailed descriptions in our Buyers Guide._
Why you need it: Patient portals are usually the MVPs—Most Versatile Players—of medical software. They automate several administrative tasks, freeing up your staff to focus on higher priority tasks. The online bill payment feature means you’ll also get paid more quickly.
Patient portals are key to a practice’s growth because patients are increasingly expecting more convenient and seamless forms of communication with their care providers. In a survey of U.S. patients, we found significant percentages of respondents being open to using these time-saving features:
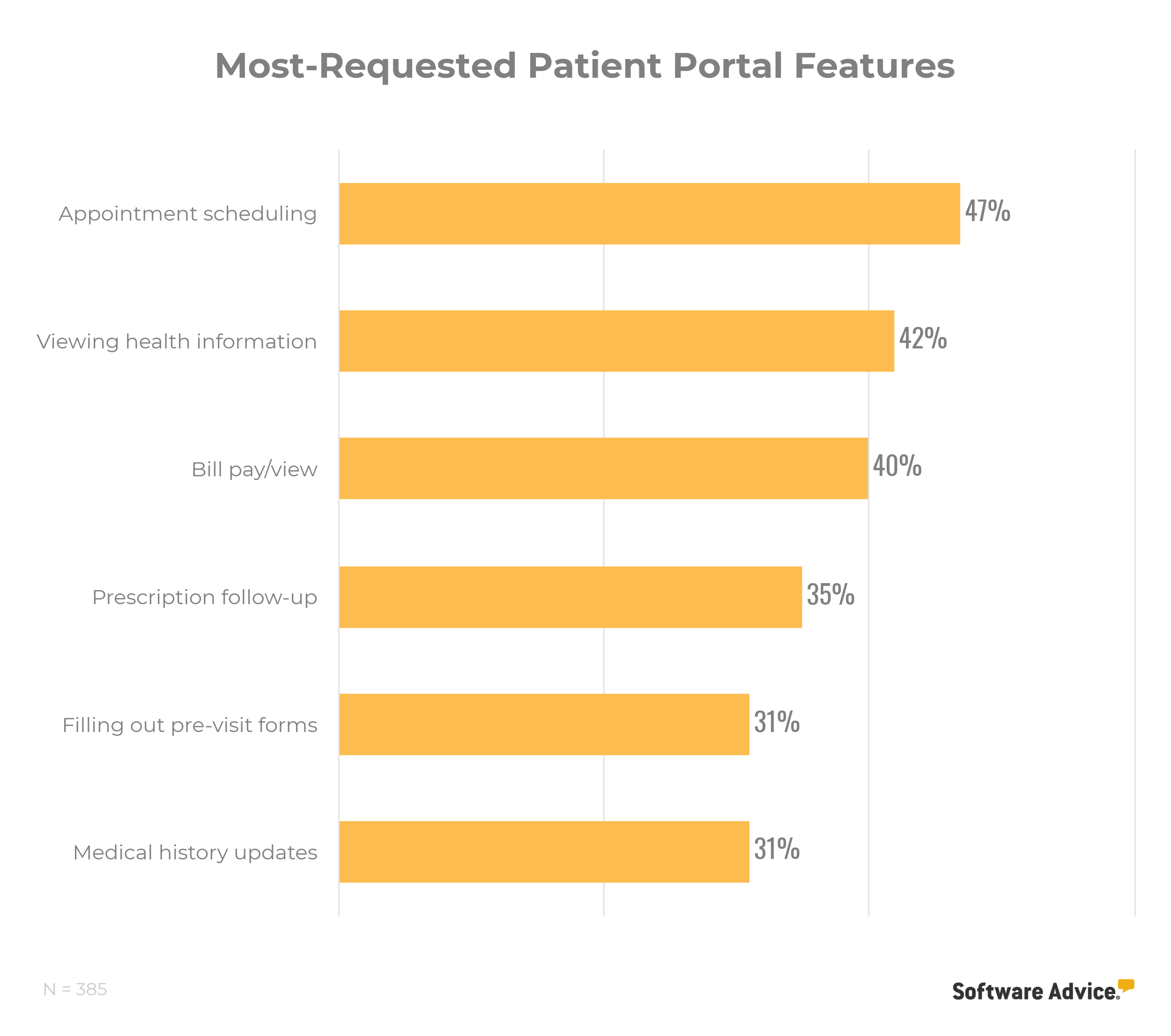
Key considerations:
Check with your EHR vendor before purchasing a stand-alone patient portal software. We found several certified EHRs that include in-built patient portals.
Before implementing a patient portal, make sure your staff is committed to actually using it and showing patients how it works. Patients hate it when you don’t answer portal messages in a timely manner or send them a link without further explanation. Your portal should be a helpful asset, not a confusing afterthought.
A significant portion of the medical software buyers we spoke with specifically called out secure, HIPAA-compliant patient-to-physician messaging when talking about their patient portal needs. If communication with patients is a struggle for you, definitely consider a patient portal system with this compliance attribute to build trust with your patients.
5. Tablet integration
What it is: Tablets (e.g., Apple’s iPad or Samsung’s Galaxy Tab) are mobile computers that let physicians access EHRs, demonstrate educational materials to patients, look up medical research, and more.
Why you need it: Desktop computers or laptops can meet all your IT needs, but they’re bulky and inconvenient to carry around. You’ll probably want a more portable alternative. As per a PatientPoint survey, 95% of physicians reported using engagement technology, such as exam room tablets or mobile apps, in some way or the other to engage with their patients.
Key considerations:
While tablets made for general consumers may suit your needs just fine, it’s worth noting that tablets specifically designed for the healthcare industry do exist. These are usually built to be sturdier and easier to disinfect than your average tablet.
It’s incredibly important to make sure that your tablet has encryption technology to prevent HIPAA violations. Read more about avoiding HIPAA violations here.
6. Speech recognition
What it is: Speech recognition software specifically designed for medical practices allows physicians to automatically transcribe their spoken words into written text. This is especially helpful when documenting clinical notes.
Why you need it: Many speech recognition solutions integrate with EHRs, so you won’t have to spend as much time typing data manually into the EHR.
As your practice grows, you’ll have less time between patient visits to finish up clinical documentation in the EHR. This software will come in handy then—allowing you to keep comprehensive records without spending long after-hours.
In a 2018 survey of more than 15,000 physicians from 29 specialties in the U.S., 56% said that too many bureaucratic tasks, such as charting and paperwork, is the top reason for burnout.
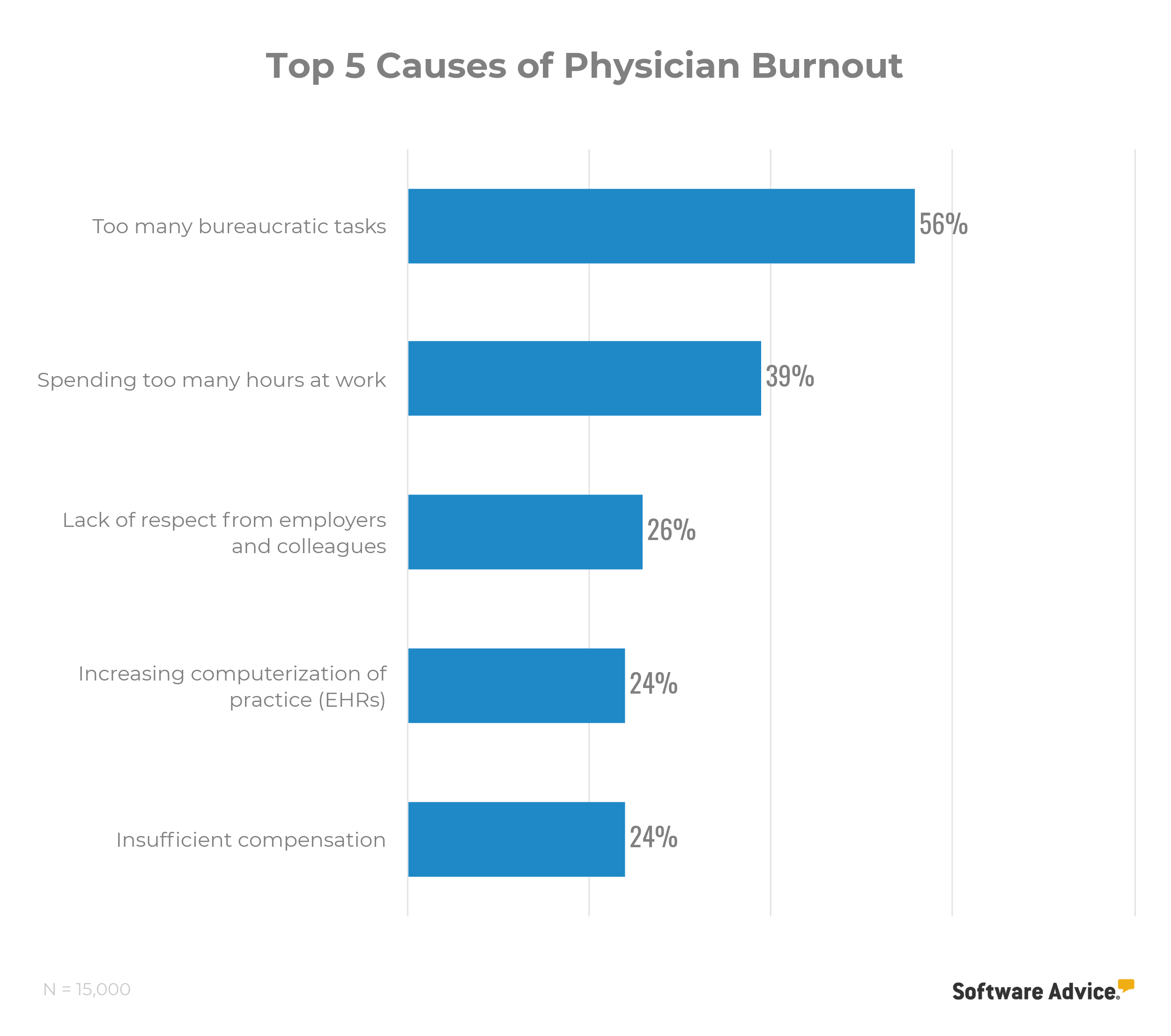
(Source)
Key considerations:
You may need to buy a separate recording device or headset to implement this technology. However, some solutions can operate with the microphone on your mobile device or laptop.
If you’re skeptical about how well these systems understand and transcribe your voice. Fear not! You can expect 95% accuracy.
Healthcare IT for optimization
This section is for established practices seeking to optimize operations by improving the processes of documenting/sharing health information and managing patient relationships.
7. Telemedicine
What it is: The term “telemedicine” refers to any technology that supports remote delivery of medical services, such as video consultations, virtual monitoring, and remote evaluations.
Telemedicine is such a multifaceted technology that it has its own Hype Cycle from Gartner (available to Gartner clients). We recommend medical practices to start by offering video consultations—the use of a video chat-enabled platform to meet with patients remotely.
Why you need it: According to Gartner, 25% of all care in the U.S. will be delivered virtually by 2020 (full report available to Gartner clients). Another survey, by MobiHealthNews, reveals that telehealth adoption and interest in the technology increased by 340% during 2015-2018.
Certain types of care will always need to be delivered in person, but the telemedicine trend is not to be ignored if medical practices want to survive tech-driven shifts in healthcare delivery.
You don’t have to wait until 2020 to start seeing the benefits of telemedicine on your practice. Video consultations allow you to expand your reach to cater to patients in remote, rural areas or in some far-away city. You can also see more patients per day and decrease the likelihood of appointment no-shows.
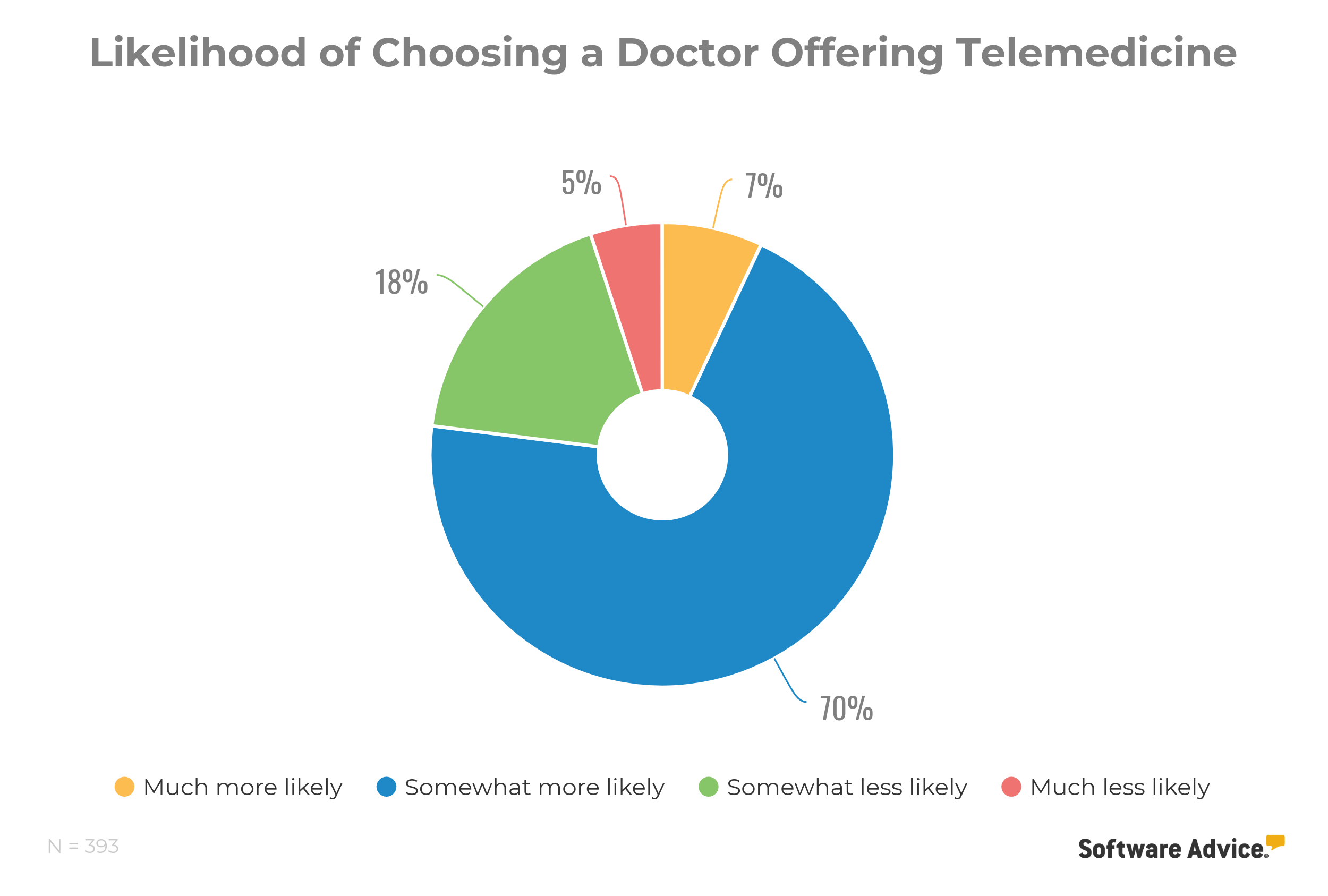
In our survey of nearly 400 U.S. patients, we found that 77% were inclined to choose a doctor over another if he/she offered telemedicine.
Key considerations:
Some EHR vendors offer integrated or add-on telemedicine functionalities, but these aren’t terribly common just yet. Check out a comparison of different telemedicine solutions—including a free one.
Depending on the platform you choose, you may have to budget for some additional upfront costs. These may include bumping up your practice’s internet speed to optimize connectivity and investing in a web camera. For more telemedicine implementation tips, click here.
8. Patient relationship management
What it is: Patient relationship management (PRM) systems, commonly known as patient engagement software or healthcare customer relationship systems, help physicians maintain frequent communication with patients (e.g., via newsletters), collect patient feedback (e.g., via satisfaction surveys), and/or manage the practice’s online presence (e.g., via social media channels).
Why you need it: In a 2018 survey of 2,002 adults in the U.S., around 38% reported switching their service provider at least twice in 2017 due to poor customer service. Patients are customers in the healthcare industry, and you should emphasize maintaining strong relationships with them to avoid losing them to another care provider.
In Gartner’s “Hype Cycle for Healthcare Providers, 2018” (full report available to Gartner clients), healthcare CRM systems received a “high” benefit ranking.
PRM systems can help you acquire and retain patients. You can check in on existing patients by sending them health screening reminders or educational materials. You can also promote your practice by launching email marketing campaigns or monitoring your reviews on sites such as Yelp.
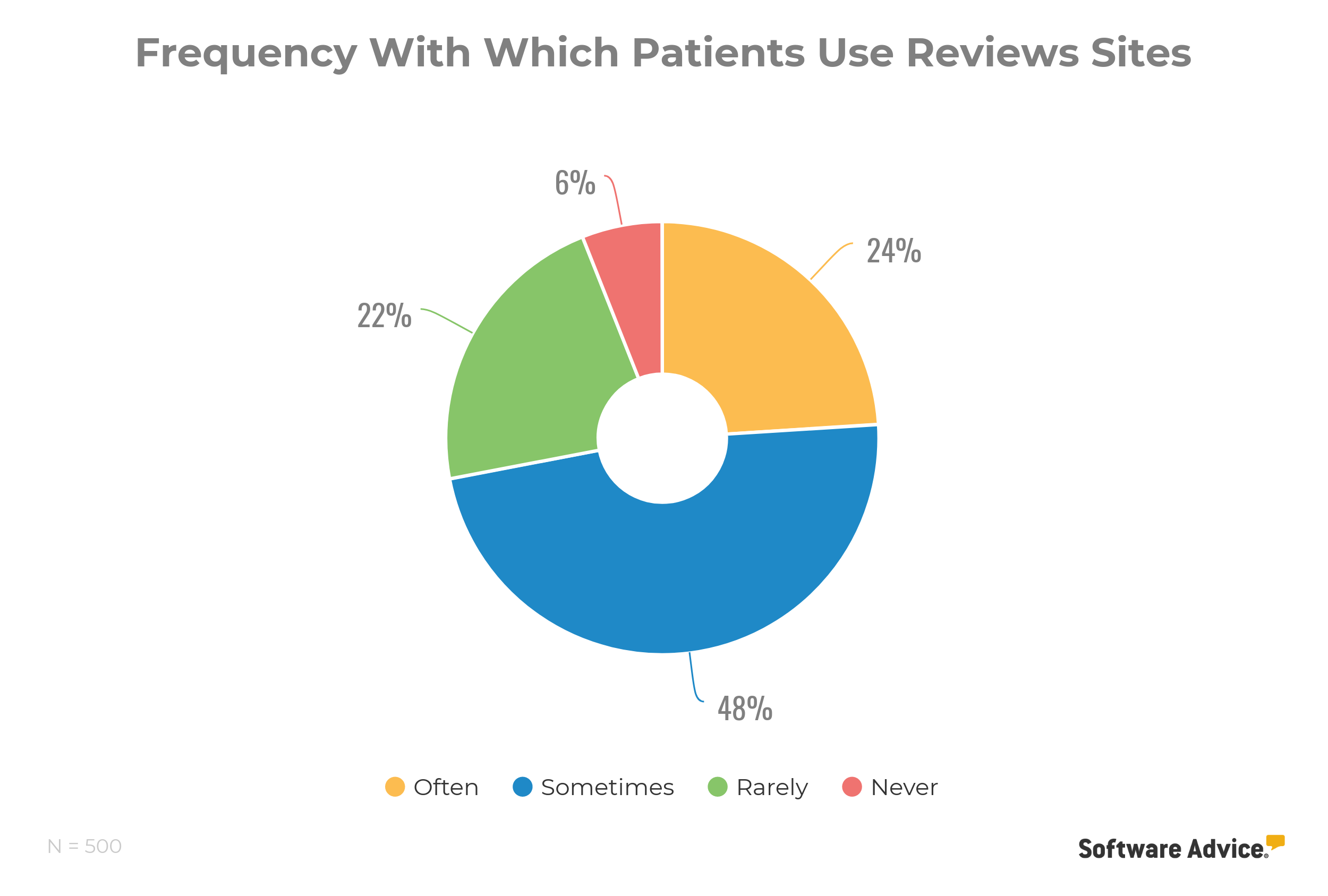
In a survey of U.S. patients, we found that 94% consult online reviews sites while choosing a doctor:
Key considerations:
EHR vendors are increasingly offering patient relationship management or patient engagement systems as add-on modules that can integrate with their clinical/practice management applications.
Make it a best practice to follow up on feedback you get on your PRM system. For example: if patients are routinely reporting too long wait times, make a plan to reduce them and update patients on your progress through email.
9. Direct messaging
What it is: Using Direct secure messaging (aka “Direct”) is like having a super-secure email address specifically designed to share sensitive health information with patients or other physicians. Practices can get a Direct address through a software vendor, a Health Information Exchange (HIE) network, or another type of Health Internet Service Provider (HISP).
Why you need it: Doctors often need to share health information with colleagues and patients, but there’s no easy way to do that. The health IT industry is still figuring out how to make EHR systems truly interoperable, which means systems from different vendors would be able to exchange patient data among themselves so authorized providers can access/interpret that data.
Your practice shouldn’t have to wait for interoperability to become a reality. You can start reaping the following benefits right now if you implement Direct to optimize your practice’s operations:

Key considerations:
Some EHRs can integrate with Direct. However, experts say the interfaces are often difficult to use and understand. If you’re not satisfied with the way your EHR vendor offers Direct technology, you can always use Direct on a separate application.
While the number of physicians using Direct is growing continuously each year, many physicians still don’t know what it is. You may need to reach out to colleagues and encourage them to get a Direct address, if you want to exchange messages with them.
Next steps
The hard part is over! Now that you know what to look for in a medical software system, it’ll be easier to assess all the options out there and make an informed decision for your practice.
If you want to save even more time, we’ve got you covered with the following resources to make software selection a breeze:
Fill out this free questionnaire. We’ll shortlist five products that meet your needs and suit your budget. Just tell us what you’re looking for, and we’ll narrow down all the products in our database at no charge to you.
Check out the FrontRunners quadrant for EMR software. This is a list of top performing solutions in the market, evaluated on value and capability scores that are powered by Gartner Methodology.
Download our free pricing guides for EHR and medical billing systems. These guides will help you understand how software is priced, what actual vendors are charging nowadays, and why you need to budget for hidden costs.
Methodology
We consulted several primary and secondary sources to choose the technologies featured in the graph, including (but not limited to) the following:
Medical practices: Software Advice has a team of software experts that provide free telephone consultations to medical practices searching for software. We studied around 4,200 of these buyer discussions (held in the last 12 months—before April 24, 2019) to gauge the demand for medical software by practice size.
Software Advice experts: We surveyed Software Advice’s team of medical software experts to vet our selections.
Gartner research: We leveraged Gartner research content, including Hype Cycle reports cited later in this guide, to help choose some of the featured technologies.