What is Patient-Centered Care, and What Does It Mean?
Many practitioners have started to realize that by focusing on their provider-patient relationships, they are also able to improve their patients' health outcomes.
Patient-centered care is a strategy that can help independent practice owners not only retain their patients, but continue to grow their practice by improving patient satisfaction and engagement.
If you've been thinking about how to focus on engaging your patients and improving your relationship with them, we'll provide you with information on how adopting a patient-centered care approach will help by explaining how it can slot into the payment model you’re already using.
And to help you determine if moving toward a patient-centered care approach is right for you and your practice, we talked to Dr. Stella Bard [1], a rheumatologist with over twenty years experience, to give us the benefits and drawbacks of patient-centered care.
Dr. Stella Bard
What is patient-centered care?
Patient-centered care is a healthcare approach that puts the patients’ health and needs at the core of every single decision that is made by the care team. It puts the emphasis on shared decision-making with all important stakeholders (the patient, nurses, caretakers, etc.) and promotes educating patients so they can make the most informed decision. Dr. Bard explains it’s key to make patients feel as though they’re “empowered to participate in their care.”
It’s a more customizable approach to healthcare compared to more traditional, rigid care models, such as fee for service, that allows the patient, their family, or caretakers control over the treatment options by providing them with research in order to help them understand their diagnosis.
Examples of patient-centered care
Patient-centered care in the doctors’ office means that you and your patient have a trusted, personal relationship. It means you have to look past a patient’s immediate symptoms and work with them to develop a care plan that works to manage or solve their underlying issues by thinking outside of just the medical diagnosis.
Dr. Bard approaches each patient-based interaction with “the understanding that they are in a vulnerable position.”
You might consider their living situation and outside stressors that can affect their health as well. This could mean referring them to peer support programs, social workers, financial counselors, mental and emotional health providers, or even helping them to find transportation.
Patient-centered care in the hospital involves patients being given the authority to identify who can visit and when. You won’t typically find strict visiting hours in a hospital that sticks to this care model. Family members (who are defined by the patient and don’t necessarily need to be blood relatives) are also active participants in the discussions and care decisions.
How does patient-centered care fit into different payment models?
Patient-centered care is a response to more traditional models of care such as fee for service which is more focused on quantifying methods of care delivery to make billing easier. While not impossible to take a patient-centered approach, the two often fight against each other because they care about different things.
In contrast, a value-based care model incentivizes your practice based on the quality of services you provide. You’re compensated depending on the patient’s health outcomes.
The goals of a value-based care system are four-fold:
Improve the quality of healthcare
Improve the patient experience
Lower costs for patients
Improve the care team’s experience
You might notice that these coincide with the goals of patient-centered care quite a bit—a patient-centered approach is crucial in a value-based care healthcare system.
It’s not the only model that works for a patient-centered approach though. Concierge medicine and direct primary care both benefit from taking a patient-centered approach.
Concierge medicine is a membership-based practice model that provides patients with more access to their healthcare provider. Patients pay a monthly or yearly subscription fee ranging from a few hundred dollars a month to thousands of dollars a month, but in turn get greater and faster access to their concierge doctor. Under some circumstances, concierge medicine can bring in health insurance.
While similar, direct primary care is slightly different: Direct primary care is a membership-based payment and practice model where patients are charged a yearly or monthly fee to gain access to a doctor instead of going through health insurance.
This is just a brief overview of some of the healthcare models that can work with patient-centered care. For a more detailed breakdown of these different models, check out these resources:
The importance of a patient-centered care model
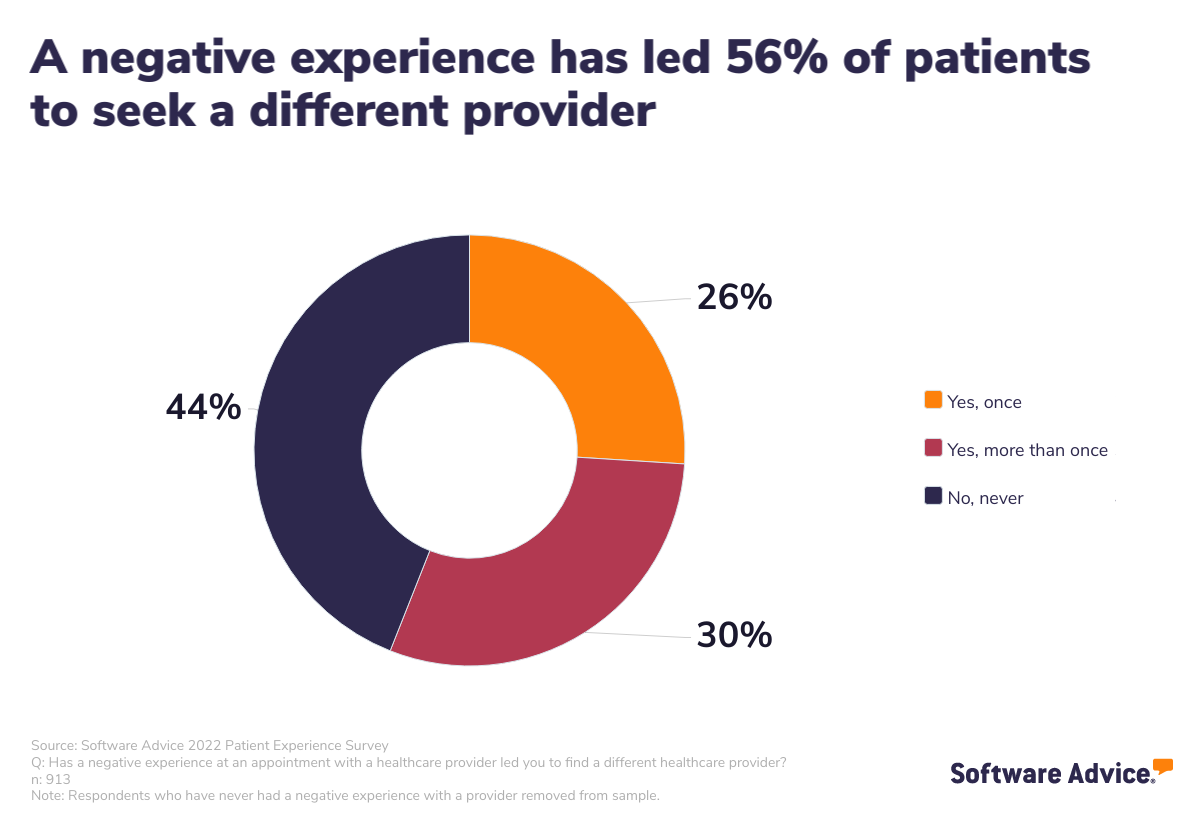
Above all, a patient-centered approach strives to improve patient health overall while simultaneously working toward improving your patients’ experience and engagement. Your patients are much less likely to have a negative experience because they are more invested in their health outcomes. According to our 2022 Software Advice Patient Experience Survey*, 56% of patients sought a new provider after having a negative experience.
By utilizing the patient-centered approach, your practice will have an inherent advantage over a practice that doesn’t since every patient coming through your doors will have an entirely different experience than they would with a more traditional care model such as fee for service.
Successful patient-centered care needs a few things:
Shared decision-making gives patients, patients’ families, and caretakers the ability to plan decisions by giving them time to research and become involved in the process before final decisions are made.
Customized care puts the patient in the middle by treating them as a unique individual who deserves to have a choice from a variety of diagnostic and treatment options.
Information sharing means the patient is presented with all observations and data the care team has gathered as well as the latest relevant condition and treatment research.
Benefits of patient-centered care
Being patient centered can benefit your healthcare organization in a variety of ways, but here, we’re going to focus on the two most important.
Creates more favorable conditions for better health outcomes
A more engaged patient will likely have better health outcomes, and a patient-centered approach helps patients learn to take control over their own health, whether it’s physical or mental health.
For example, Dr. Bard has found that a patient that “is left feeling heard, with their values respected, are more informed and therefore, more empowered. This leads to better health outcomes, with faster recovery, less ER visits, and decreasing use of healthcare resources.”
A patient who’s engaged with their care plan is more likely to take their medications as prescribed as well as self-manage their temporary or chronic conditions because they have a far greater understanding of why they’re doing these things to begin with.
By encouraging practitioners to focus on providing personalized solutions to each patient’s underlying health issues, patient-centered care helps achieve better outcomes in the long run. It incentivizes doctors to be more thoughtful about what they prescribe and how they approach each patient. It also ensures physicians recommend only the most needed services, saving patients money on unnecessary tests or procedures.
If you want more information about patient engagement and how it can help improve your practice, check out these resources:
Improves patient satisfaction
You might think that focusing on patient experience or engagement is enough, but patient satisfaction is an oft overlooked aspect of improving health outcomes for patients.
Patient experience and patient satisfaction are often used interchangeably, but they’re not quite the same thing. Patient satisfaction differs from patient experience because patient satisfaction is about whether or not their expectations have been met; it’s more about patient perception.
You might provide the exact same level of patient experience to two patients experiencing very similar issues, but one might leave very satisfied while the other might leave less satisfied because their expectations are different.
Because patients are more involved in their health outcomes, they’re more likely to engage with the doctor. This means both the doctor and the patient are more likely to leave each engagement with higher satisfaction.
During initial consultations, doctors and nurses spend time with their patients to get a more holistic idea about the reason for their visit. This improves the care experience for patients, as their needs are personally attended to.
Patient-centered care cuts straight to what patient satisfaction is all about by engaging with each individual patient’s expectations for their care service and molding your approach to their expectations. This practically guarantees that every patient will be satisfied with their care.
If you’re looking for other ways to improve patient experience or gauge patient satisfaction, check out these resources:
Drawbacks of patient-centered care
Patient-centered care can take some effort to get up and running, so it’s important to have a clear understanding of the drawbacks that come up whenever you’re making the switch.
It can be an expensive model to get started
It can be tough knowing where to start when you’ve only ever used a more traditional healthcare delivery model, and you’re not the only one to feel those stresses. After all, the healthcare industry is largely set up to enable those entrenched systems—for example, most software is designed around it.
Dr. Bard even cites this as one of the complications that can arise from adopting a patient-centered approach: “It's expensive and time consuming for the physician and requires many resources initially to get it started.”
It’s not impossible though, and if you’re in the process of setting up a new practice or going in with a few other physicians to start a medical practice partnership, you’re in a great position to design your practice with a patient-centered approach from the get-go. To this end, you’ll want to emphasize software and technology that enables communication with patients.
The cost can be daunting, but as long as you’re intentional when it comes to the software and tech choices you make early on, you’ll be rewarded with the benefits that a patient-centered care approach offers.
Some patients might push back at being an active participant in their health
The simple truth of the matter is that some patients might not be a good fit for patient-centered care. Because it goes against the grain, some patients might be surprised to find out that they have more agency in their health, and many patients will have never experienced that before. While some might find this new agency freeing, others might find it stifling and overwhelming.
In fact, Dr. Bard confirmed that “some patients prefer not to be ‘burdened’ with making their own decisions about their health and prefer the patriarchal model where they are told what to do by the expert and professional."
You should be prepared to offer educational resources about the benefits of having more control over their health for patients who might be skeptical, and your staff should also be knowledgeable about how to engage with patients who might be hesitant.
With more hesitant patients, do your best to educate and inform, but if a patient isn’t willing to meet you halfway, nobody is being served by continuing the relationship. In those cases, it might be best for you to refer them to a more traditional colleague who will be a better fit.
Resources needed to transition to a patient-centered approach
The requirements of a patient-centered care doesn’t differ too much from a traditional practice. You’ll still need the standard tech you’d find in most practices:
Electronic health record (EHR) software helps you keep detailed notes about your patients’ health history as well as their personal lives in order to have a more complete picture of their problems. Additionally, with the increased focus on interoperability, you’ll have a better understanding of their long-term health history if your EHR is interoperable.
Patient portal software allows your patients and their caretakers to take more ownership of their care plans because it has all of the relevant, important information in one place that is easily accessible via mobile devices. Patient portals also allow more fluid communication between patients and doctors because your patients can send questions directly from the patient portal.
Patient scheduling software works to help you decrease no-shows and increase staff efficiency by reducing the number of repeatable, menial tasks. If your staff doesn’t have to manually schedule each appointment over the phone, that frees them up to focus on patients who are currently in the office and need assistance. It’s a win-win for patients as well because they can schedule appointments at any time of the day from any mobile device or computer.
But, as a patient-centered care practice, you might also want to look into more specific technologies such as care management software, or more specialized patient engagement software.
The important thing to remember whenever you’re vetting and researching tech and software is that the goal of patient-centered care is to provide the most effective and efficient communication between you and your patients. Utilizing technology can help you implement patient-centered care more effectively by streamlining provider-provider and patient-provider communication which will lead to better overall relationships.
Effective communication is vital for the patient-provider relationship because it helps you garner trust, gather better healthcare data, and support patients when and wherever they need it—having technology in place which efficiently enables this goes a long, long way.
For more information about the ways that technology can help your practice grow, check out these resources:
Tech can only get you so far
Despite all that we just told you, it’s important to also remember that technology can only get you so far. You need to make sure that you and your staff are properly trained on the soft skills necessary for a successful patient-centered approach.
Because patient-centered care is, at its core, about communication, you need to know how to best communicate with each patient. Every one of your patients will want to be communicated with in a different way. The types of communication will be different which will change the approach you need to take to best serve them. This requires a lot of emotional intelligence from not just you but also your entire staff.
That’s why your first appointment with each patient should focus nearly entirely on setting up best practices. You need to have a detailed conversation about the best way to communicate, offer feedback, or present options to them. What kind of information do they find most important? How do they want to be communicated with? Email, text, phone
Symptoms and diagnosis are vitally important, but because you’re building a lasting, personal relationship with each patient, you need to treat it as such and build a solid foundation.
Patient-centered care is trending to be the future of healthcare
At its core, patient-centered care is about making sure each of your patients are given the information and urgency to take more agency over their own health in a system that, traditionally, doesn’t incentivize or allow them to do so. Patient-centered care means you must understand that your patients are often in vulnerable positions, so you have to consider their social, emotional, and financial situations and how they might relate to their health.
That’s why practice owners and admins who implement more patient-centered care strategies are more likely to retain and attract patients who are fed up and disenfranchised with the way our healthcare system typically operates. Not only will you build lasting provider-patient relationships, but you’ll be helping transform the healthcare industry for the better.
With the push toward more value-based healthcare, now is the time to make the switch since more and more resources are becoming available to smaller healthcare organizations.
Survey methodology
* Software Advice's 2022 Patient Experience Survey was conducted online in October 2022 among 1,001 respondents in the U.S. Respondents were all adults who had visited a healthcare provider within the past three years.