Best Construction Categories
Best Facilities Management Categories
Best Human Resources Categories
Best Legal Management Categories
Best Manufacturing Categories
Best Medical Categories
Best Property Management Categories
Get 1-on-1 advice in 15 minutes. It's free.

Josh P.

AI Tools in Healthcare Software: Top 5 Must-Have Features
Discover five AI features that can save hours of charting, improve clinical decisions, and streamline patient communication, so your practice runs smarter, not harder.
If you're staying past 7 PM to finish charting, you're not alone. Most physicians spend half their valuable time on documentation instead of seeing patients.
AI tools in healthcare are changing that, helping medical practices cut charting time and focus on what matters most: better outcomes. Our latest survey* found that AI applications are the number #1 planned software purchase for medical practices. But what are the best AI solutions transforming healthcare practices? How do you find the best fit for your workflow?
Here's the problem: not all AI features deliver on their promises. Some create more work than they save.
The workaround: After analyzing usage data from successful software adopters, here are five AI features that medical practices are using successfully to reduce administrative burden and help with clinical decisions.
We'll show you what each feature does, the associated benefits, and what to look for when evaluating vendors.
1. NLP for clinical documentation (AI scribe)
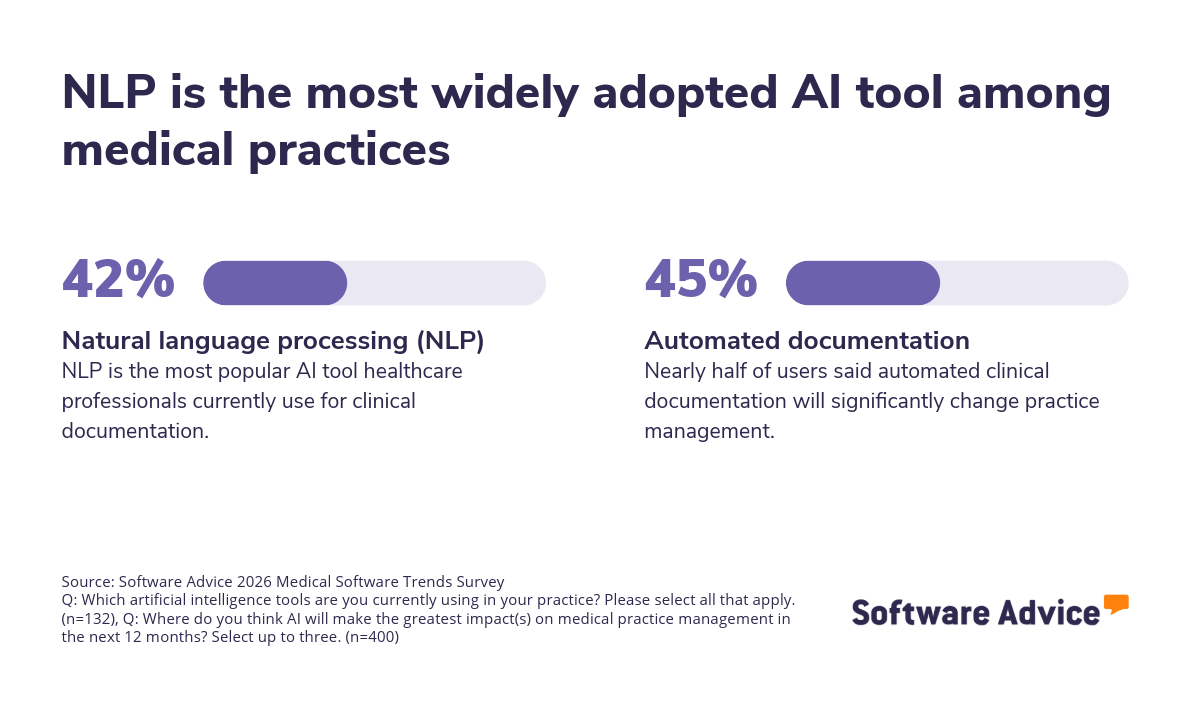
Natural language processing (NLP) powered documentation tools (also called AI scribes) listen to patient encounters and automatically generate clinical notes, reducing the time providers spend on paperwork.
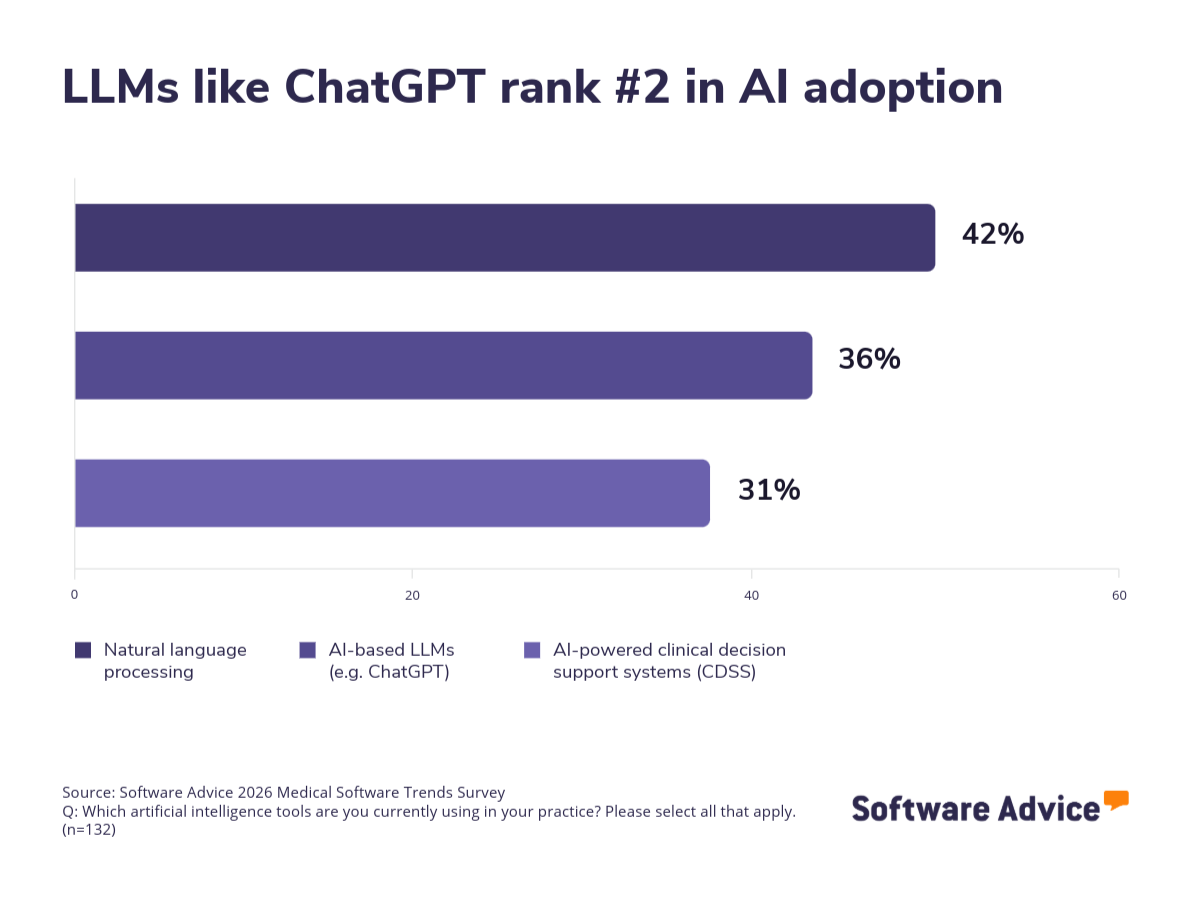
This is the most widely adopted AI application for medical practice management among surveyed physicians.
Benefits: Cuts time spent on charting, improves accuracy, and supports comprehensive insurance documentation.
What to look for in this feature:
Specialty-specific terminology: The system should understand the vocabulary and documentation patterns specific to your practice type.
Review workflow: Look for interfaces that make it simple to review, correct, and approve AI-generated notes before they're finalized.
Compatibility with your EHR: Ensure the platform can transfer documentation into your existing electronic medical record system without needing you to copy-paste.
Ambient vs. dictation modes: Ambient systems capture natural conversation; dictation requires you to speak directly to the software. Choose the preferred feature based on your style.
Confidence indicators: The best systems flag sections where they've misheard or misinterpreted (due to unclear medication names or complex medical terminology), prompting human review.
HIPAA compliance: Confirm encryption and secure data storage in accordance with applicable laws.
Questions to ask vendors
How does the system handle multiple speakers in a room?
What happens when it encounters unfamiliar terminology?
What's your error rate for clinical accuracy, and how do you measure it?
Is the AI trained on data from practices similar to mine?
2. AI-powered clinical decision support systems
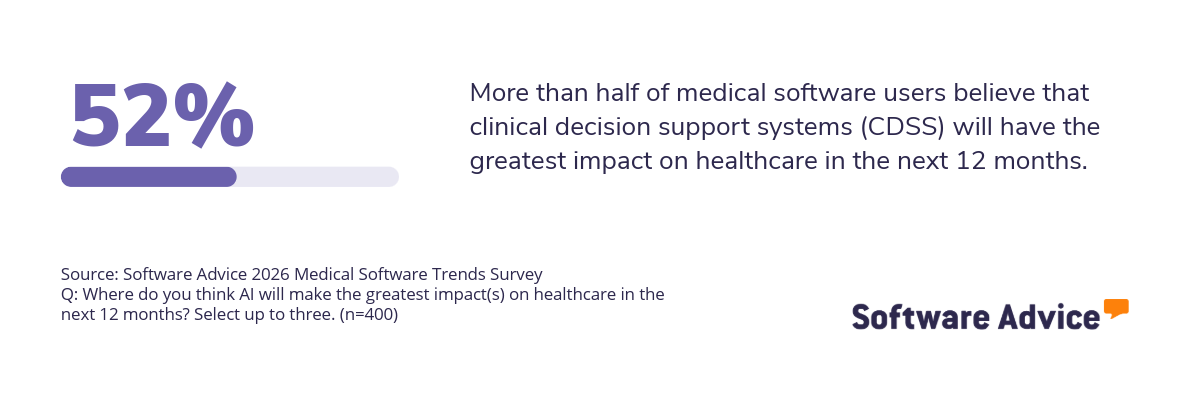
Over half of providers believe clinical decision support systems (CDSS) will make the greatest impact on healthcare in the next year.
Among current AI users, 31% already rely on AI-powered CDSS, making it one of the top three applications in active use.
Benefits: CDSS can detect drug interactions, flag abnormal lab values, and recommend evidence-based treatment protocols, serving as a safety net for busy clinicians. Moreover, it reduces the time spent researching clinical guidelines during patient visits.
What to look for in this feature:
Explainable recommendations: The system should provide clear explanations for its suggestions, citing relevant clinical guidelines, research, or specific patient data points, rather than relying on opaque outputs.
Adjustable sensitivity: You should be able to tune alert thresholds to prevent alert fatigue while maintaining safety.
Patient context integration: Recommendations should account for the patient's full history, current medications, allergies, and conditions; not just the immediate issue.
Up-to-date evidence: The system should regularly update itself with the latest clinical guidelines and research.
Confidence scoring: Look for systems that indicate how certain they are about a recommendation.
Questions to ask vendors
What clinical guidelines and evidence sources inform your recommendations?
How often is your knowledge base updated?
Can you show me examples of how the system explains its reasoning?
Do you monitor false positive rates for alerts?
Can I customize alert settings to match my practice patterns?
3. AI-powered virtual assistants and chatbots for patient communication
Virtual AI assistants take routine tasks off your plate, handling scheduling, refills, and patient queries—so your team can focus on care, not the front desk.
These can also triage, through text, voice, or chat interfaces.
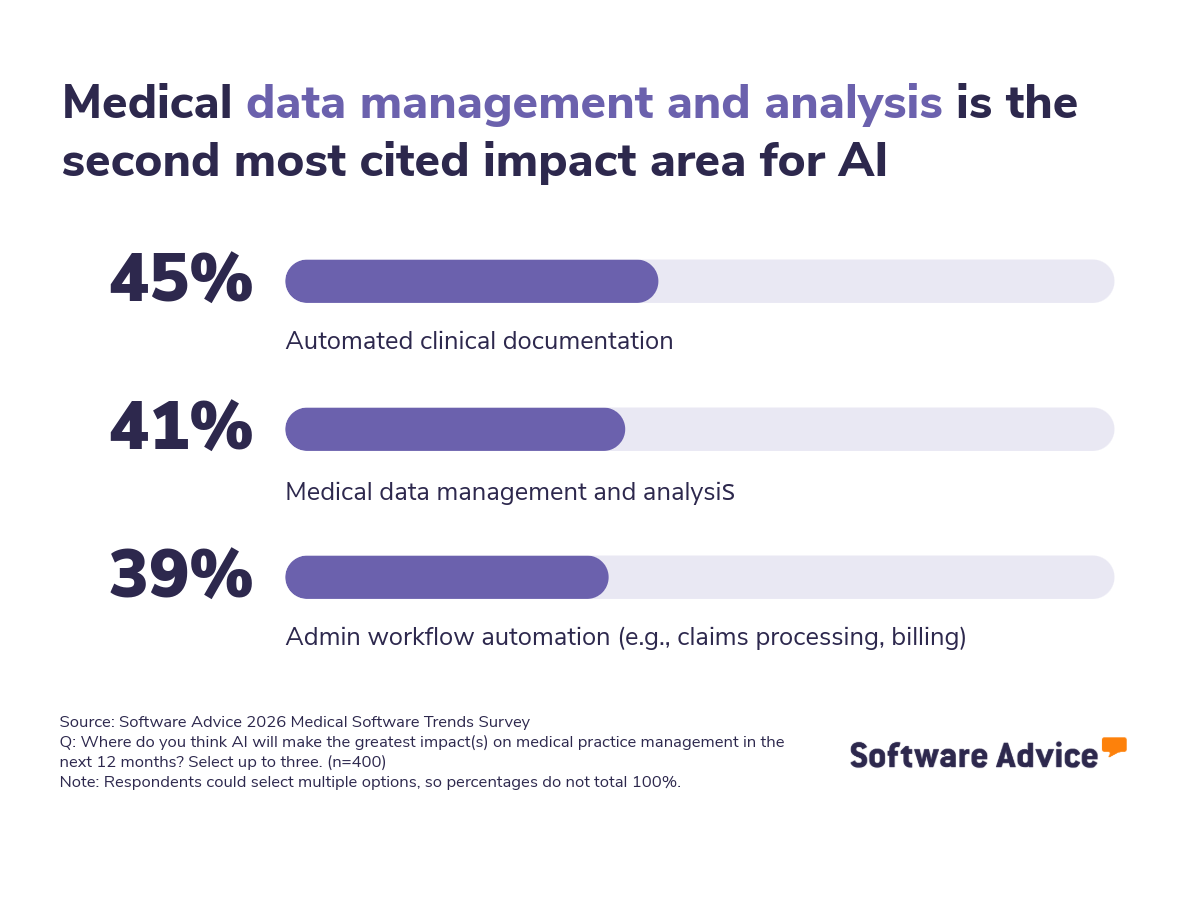
Our survey revealed that virtual appointments are now averaging 17% of patient visits for medical professionals. Currently used by 30% of medical practices, virtual healthcare AI agents directly address one of the biggest pain points for small practices in healthcare: overwhelming administrative workload at the front desk.
Benefits: Improves patient experience and reduces front-desk workload, freeing staff for more complex patient needs.
What to look for in this feature:
Smart routing and escalation: The system should recognize when it's out of its depth and seamlessly transfer to a human staff member with context.
Appointment optimization: Goes beyond simple scheduling to suggest optimal times based on appointment type, provider availability, and even no-show risk.
Clear AI identification: Patients should know they're interacting with AI, not a person.
Easy human handoff: Patients can reach a real person at any point without frustration.
HIPAA compliance: Ensure conversations are encrypted and stored securely, with appropriate access controls.
Questions to ask vendors
How does the system handle angry or confused patients?
What percentage of conversations require human escalation?
How do you handle protected health information in conversations?
Can I review conversation logs and provide feedback to match our practice culture?
4. AI-based large language models for admin tasks
36% of medical software users already use AI-based large language models (LLMs) like ChatGPT in their practice, the second-highest adoption rate after NLP for documentation.
These large language model (LLM) tools have quickly become part of many practices' workflows, and assist with tasks like drafting patient communication, summarizing research, and even administrative writing. However, their general-purpose nature requires more careful evaluation than medical-specific AI. However, their general-purpose nature requires more careful evaluation than medical-specific AI.
Benefits: Saves time on administrative writing tasks, helps translate complex medical concepts into simple terms for patients, and provides a flexible tool for various non-clinical workflows.
What to look for in this feature:
Medical-specific vs. general-purpose: Decide if you need LLMs trained on medical literature (more accurate for clinical content) or general models (more flexible for admin tasks).
Integration vs. standalone: Some medical software embeds LLM capabilities, while others require separate tools. Integration reduces the need for copying sensitive data between systems.
Clear usage policies: Since LLMs are flexible, you need guidelines on appropriate vs. inappropriate uses in your practice.
Privacy controls: Ensure you have agreements that prevent your sensitive data from training future models, and use business or enterprise versions.
Fact-checking mechanisms: More sophisticated models will include citation features or confidence indicators for medical claims.
Questions to ask vendors
What LLM powers this feature, and is it trained on medical data?
How do you prevent the AI from generating false medical information or hallucinations?
What data privacy protections are in place?
How do you handle bias in AI outputs?
Keep in mind: Always independently verify clinical or patient-facing LLM outputs. LLMs can confidently generate false information; therefore, always vet the content before using it in patient care, billing, or communication.
5. AI for medical data analysis and management
AI turns raw patient data into actionable insights, helping you predict risks, optimize schedules, and improve care without hiring a full-time analyst.
Data management and analysis is the second most common way AI could impact medical practice management, according to survey respondents. As practices accumulate more data but lack dedicated analysts, AI fills the gap between having data and using data effectively.
But here's the challenge: AI is only as good as the data you feed it. ‘High-quality data for AI systems’ ranks as a top implementation challenge, meaning many practices have inconsistent documentation that undermines AI effectiveness.
Benefits: AI-powered analysis tools can help uncover patient trends, predict risks, optimize scheduling, and flag incomplete documentation.
What to look for in this feature:
Actionable insights, not just dashboards: Look for AI tools that suggest specific actions ("Call these 15 high-risk diabetic patients overdue for tests") rather than just showing graphs.
Automated data quality checks: Systems that identify missing information, inconsistencies, or errors in records before they cause problems.
Explanations for predictive analytics: No-show predictions, readmission risks, or population health insights should explain which factors drive predictions.
Anomaly detection: Flags unusual patterns that might indicate coding errors, fraud, or clinical concerns.
Integration with existing systems: Should pull records and data from your EHR/EMR, practice management system, and billing tool without manual data exports.
Questions to ask vendors
How do you ensure data quality before analysis?
Can you show me examples of actionable insights your system generates?
How do you validate that your predictions are relevant and accurate for practices like mine?
What ongoing data maintenance is required to keep the system effective?
Test before you commit!
Our survey data shows that physicians are eager for AI solutions, with adoption accelerating across documentation, decision support, and data management. But the same professionals also understand the risks. Over-reliance on AI, data quality challenges, and skills gaps are all real concerns shared.
Success with AI isn’t about being first, it’s about being smart and deliberate.
Start with one AI feature that addresses your biggest pain point. Test it thoroughly, train your team properly, and then expand.
Before purchasing:
Demand 30-day trials with real patients and real workflows (demos are theater, trials are truth)
Verify security obsessively (SOC 2 reports, breach insurance, specific data storage locations)
Read user reviews and take expert advises (not just vendor-provided references, find them in rating sites or forums)
Budget 3x the training time providers estimate (staff adoption determines ROI, not feature lists)
By asking the right questions and building in the right safeguards, you can adopt AI in ways that genuinely improve your practice.
Need help choosing the right AI-enabled feature for your medical practice? Our advisors can help you compare options based on your specific needs, budget, and current systems. Schedule a free consultation or chat now with a Software Advice advisor.
Related readings:
5 Key Medical Practice Management Software Features With Top Products That Offer Them
Top 10 Medical Practice Management Software With AI-Enabled Features
Everything You Need To Know About Medical Practice Marketing
Patients Want Fast Care from Corporate Practices, but Trust Independent Practices More
Everything You Need To Know Before Starting a Medical Practice Partnership
Survey methodology
*Software Advice 2026 Medical Software Trends Survey was conducted online in September 2025 among 400 physicians in the U.S. employed full-time in medical practices. The goal of this study was to understand the timelines, organizational challenges, research behaviors, and adoption processes of medical software buyers. Respondents were screened to ensure their involvement in medical software purchasing decisions. The study included 134 small practices (1-5 licensed providers), 144 medium practices (6-20 licensed providers), and 122 large practices (more than 20 licensed providers).